Atrial Septal Defect (ASD) is one of the most common congenital heart defects (CHD), accounting for approximately 10% of all CHD cases. This defect, characterized by an abnormal opening in the atrial septum, allows blood to shunt between the atria, leading to volume overload, right heart enlargement, and potential pulmonary hypertension if left untreated.
For pediatric cardiac surgeons, perfusionists, and healthcare providers, understanding the latest diagnostic techniques, surgical advancements, and postoperative care strategies is essential to optimize patient outcomes. This guide delves into the intricacies of ASD, covering its classification, symptoms, diagnosis, treatment modalities, and long-term management.
Understanding Atrial Septal Defect (ASD)
Types of ASD
ASDs are classified based on their location in the atrial septum:
- Secundum ASD: The most common type (70%), occurring in the central portion of the septum near the fossa ovalis.
- Primum ASD: Located in the lower atrial septum and often associated with atrioventricular (AV) septal defects.
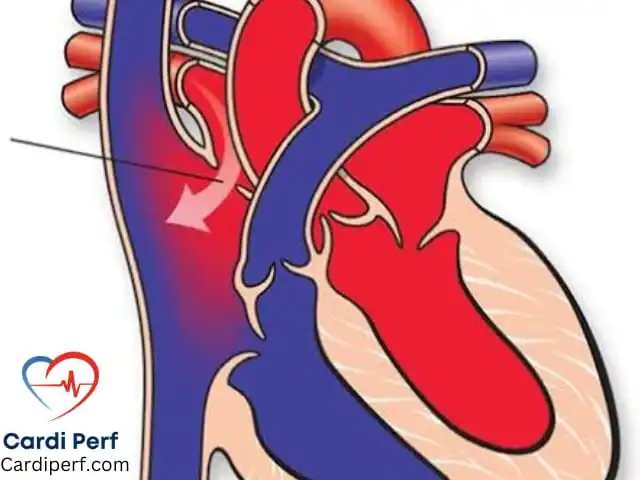
- Sinus Venosus ASD: A defect near the superior vena cava (SVC) or inferior vena cava (IVC), often linked with anomalous pulmonary venous return.
- Coronary Sinus ASD: A rare variant where the coronary sinus is partially or entirely unroofed, allowing shunting into the left atrium.
Clinical Presentation and Symptoms
ASD symptoms vary based on defect size and associated conditions:
- Small ASDs (<5 mm): Often asymptomatic and may close spontaneously.
- Moderate to Large ASDs (>6 mm): Symptoms may include:
- Recurrent respiratory infections
- Fatigue and exercise intolerance
- Palpitations due to arrhythmias (e.g., atrial fibrillation or flutter)
- Signs of right heart failure in untreated adult patients
Late complications in untreated cases include pulmonary hypertension, right ventricular dysfunction, stroke due to paradoxical embolism, and Eisenmenger syndrome.
Diagnosis of ASD
Echocardiography (Primary Diagnostic Tool)
- Transthoracic Echocardiography (TTE): First-line imaging modality, especially in pediatric patients.
- Transesophageal Echocardiography (TEE): Provides detailed assessment, particularly in adult patients or before transcatheter closure.
- Bubble Contrast Study: Detects right-to-left shunting and risk of paradoxical embolism.
Other Diagnostic Modalities
- Cardiac MRI and CT Angiography: Used for complex ASDs or suspected pulmonary venous anomalies.
- Electrocardiography (ECG): May show right atrial enlargement, right bundle branch block, or atrial arrhythmias.
- Cardiac Catheterization: Performed in select cases to assess pulmonary pressures and shunt fraction (Qp/Qs ratio).
Treatment Modalities for ASD
1. Watchful Waiting for Small ASDs
- Spontaneous closure is common in defects <5 mm in early childhood.
- Regular follow-up with echocardiography is recommended.
2. Transcatheter ASD Device Closure (Minimally Invasive Approach)
- Preferred for secundum ASDs (6-25 mm) with adequate rim tissue.
- Devices Used:
- Amplatzer Septal Occluder
- Gore Cardioform Septal Occluder
- Procedure Overview:
- Performed via cardiac catheterization under fluoroscopic and echocardiographic guidance.
- The device is deployed across the defect, sealing the abnormal opening.
- Post-procedure monitoring ensures proper placement and function.
- Advantages:
- Shorter hospital stay
- Reduced complications
- Faster recovery and minimal scarring
- Contraindications:
- Primum, sinus venosus, or large secundum ASDs without sufficient rims.
3. Role of the Pediatric Cardiologist
- Diagnosis & Assessment:
- Pediatric cardiologists play a crucial role in detecting ASDs early using non-invasive imaging techniques.
- Determining the Best Treatment Plan:
- They evaluate the size, location, and hemodynamic impact of the defect to recommend closure strategies.
- Long-Term Follow-Up:
- ASD patients require continued monitoring for arrhythmias, right heart function, and residual shunts.
- Pediatric cardiologists manage exercise restrictions and lifestyle recommendations.
4. Surgical ASD Repair
- Indicated for large defects (>25 mm), primum ASDs, sinus venosus ASDs, or associated anomalies.
- Minimally Invasive ASD Repair:
- Robotic-Assisted ASD Closure: Utilizes robotic arms for precise movements with minimal incisions.
- Right Mini-Thoracotomy Approach: Provides excellent cosmetic outcomes with reduced pain and faster recovery.
- Surgical Techniques:
- Primary Closure: Direct suture closure for small defects.
- Pericardial or Dacron Patch Closure: Used for larger ASDs.
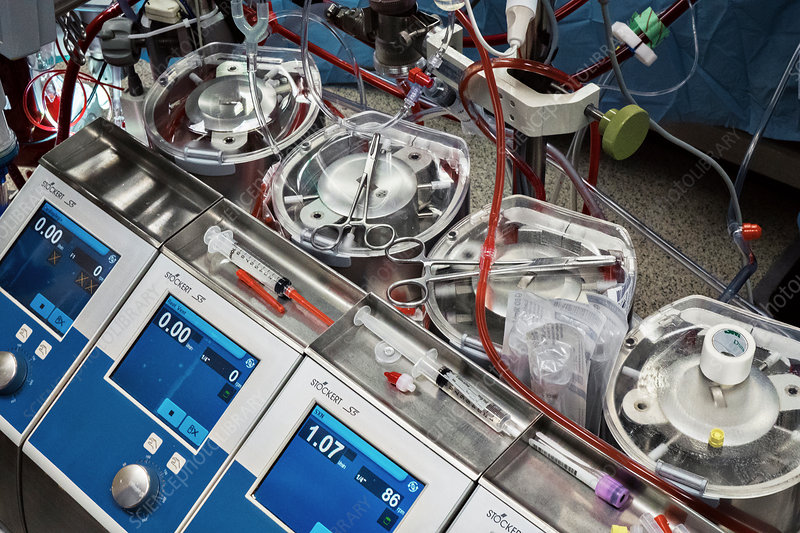
- Cardiopulmonary Bypass Considerations:
- Perfusion strategies aim to maintain normothermia or mild hypothermia.
- Aortic and bicaval cannulation is standard.
- Cross-clamp and myocardial protection protocols vary based on institutional practices.
FAQs About Atrial Septal Defect (ASD)
- What causes ASD?
- ASD is a congenital defect that occurs due to improper closure of the atrial septum during fetal development.
- Can ASD close on its own?
- Small ASDs often close spontaneously within the first few years of life, but larger defects usually require intervention.
- How is ASD diagnosed?
- Diagnosis is typically made using echocardiography, supplemented by ECG, MRI, or cardiac catheterization in complex cases.
- What are the risks of untreated ASD?
- Long-term risks include pulmonary hypertension, heart failure, arrhythmias, and paradoxical embolism leading to stroke.
- What are the treatment options for ASD?
- Treatment ranges from watchful waiting for small defects to transcatheter device closure or surgical repair for larger ASDs.
- How does transcatheter closure work?
- A catheter is inserted into a vein and guided to the heart, where a closure device is deployed to seal the defect.
- What is the role of a pediatric cardiologist in ASD management?
- Pediatric cardiologists diagnose, monitor, and determine the best treatment plan for ASD patients, ensuring long-term cardiac health.
- What is the recovery time after ASD surgery or device closure?
- Most patients recover from transcatheter closure within a few days, while surgical repair may require a few weeks.
- Can ASD lead to other heart problems such as arrhythmias or stroke?
- Yes, ASD increases the risk of atrial arrhythmias and paradoxical embolism, which can cause stroke.
- Is ASD hereditary, and can it be prevented?
- There is a genetic component, but it cannot always be prevented. Genetic counseling may be recommended for families with a history of CHD.
Conclusion
Atrial Septal Defect (ASD) is a prevalent congenital heart defect with a wide spectrum of clinical presentations and treatment options. Advancements in transcatheter device closure, minimally invasive surgery, and perfusion strategies have significantly improved outcomes for patients of all ages. for updated information visit us at cardiperf.com