We delve into the complexities of managing pulmonary embolism (PE) —a life-threatening condition that demands collaboration among perfusionists, cardiac surgeons, intensivists, cardiac anesthesiologists, and cardiologists.
Whether you’re looking to deepen your understanding of PE management or seeking practical tools for your practice, this guide has you covered. Let’s dive in!
Understanding Pulmonary Embolism: What You Need to Know
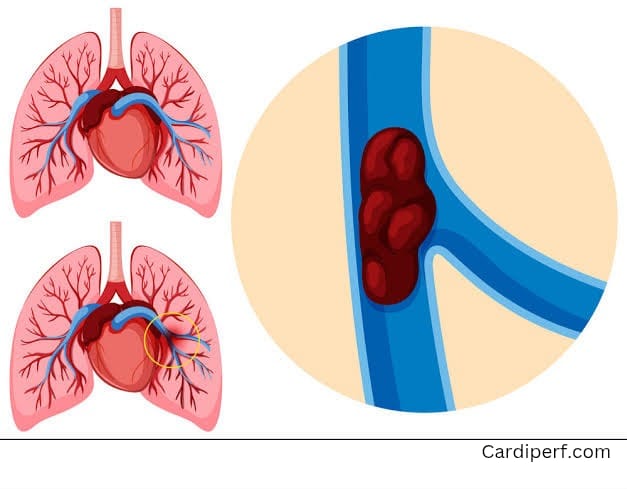
What Is Pulmonary Embolism?
Pulmonary embolism (PE) occurs when a blood clot blocks one or more arteries in the lungs. While some cases are mild, others can lead to right ventricular (RV) dysfunction , hemodynamic instability, or even death.
- Submassive PE : Characterized by RV dysfunction without systemic hypotension.
- Massive PE : Associated with hemodynamic collapse and requires immediate intervention.
Early identification and risk stratification are critical to preventing complications.
Risk Stratification Tools
To assess the severity of PE, healthcare providers rely on tools like:
- PESI (Pulmonary Embolism Severity Index) : Predicts 30-day mortality based on clinical variables.
- sPESI (Simplified PESI) : Focuses on key predictors like age, heart rate, and oxygen saturation.
- Biomarkers : Elevated troponin or BNP levels indicate myocardial stress and RV dysfunction.
These tools help guide treatment decisions, ensuring timely interventions.
The Role of Multidisciplinary Care: Introducing PERT Teams
What Is a PERT Team?
A Pulmonary Embolism Response Team (PERT) brings together specialists from multiple disciplines to manage complex PE cases. This collaborative approach ensures patients receive the most appropriate treatment based on their clinical presentation.
Key Members of a PERT Team
- Cardiac Surgeons : Advocate for surgical embolectomy in cases with large central clots.
- Intensivists : Manage ICU-level care, including mechanical ventilation and vasopressor support.
- Cardiac Anesthesiologists : Ensure hemodynamic stability during high-risk procedures.
- Cardiologists : Guide pharmacologic therapies like anticoagulation or thrombolysis.
- Perfusionists : Play a pivotal role in managing cardiopulmonary bypass during surgery or initiating ECMO support.
By leveraging the expertise of each specialty, PERT teams streamline decision-making and improve outcomes.
Interventional Strategies for Managing PE
1. Anticoagulation Therapy
Anticoagulation remains the cornerstone of PE management. Common options include:
- Heparin
- Low-molecular-weight heparin (LMWH)
- Direct oral anticoagulants (DOACs)
While effective for many patients, anticoagulation alone may not suffice in cases of submassive PE with significant RV strain.
2. Catheter-Directed Thrombolysis (CDT)
Catheter-directed thrombolysis delivers low-dose thrombolytic agents directly to the clot, reducing the risk of bleeding compared to systemic thrombolysis.
- Benefits :
- Reduces thrombus burden.
- Improves RV function.
For cardiologists and intensivists, familiarity with CDT devices and protocols is essential.
3. Percutaneous Mechanical Thrombectomy
Mechanical thrombectomy devices, such as the AngioVac or Penumbra system, allow minimally invasive removal of thrombus. These are particularly useful for patients with contraindications to thrombolysis.
4. Surgical Embolectomy
Surgical embolectomy involves direct removal of clot from the pulmonary arteries. Modern techniques have improved outcomes, but careful planning is required to ensure complete clot extraction.
5. Extracorporeal Membrane Oxygenation (ECMO)
ECMO provides temporary circulatory and respiratory support in cases of hemodynamic collapse.
- Types of ECMO :
- Venoarterial (VA) ECMO : Supports both cardiac and respiratory functions.
- Venovenous (VV) ECMO : Primarily supports oxygenation.
Perfusionists play a critical role in initiating and maintaining ECMO support.
Case Study: Managing Submassive PE with a Multidisciplinary Approach
Presentation
A 56-year-old man with recent trauma presented with acute shortness of breath. Imaging revealed submassive saddle PE with RV strain on echocardiography. Despite these findings, the patient was clinically stable.
Management
The PERT team recommended:
- Conservative management : Initiation of heparin therapy.
- Precautionary measures : Placement of femoral cannulae for potential ECMO support.
- Close monitoring : Admission to the ICU with serial echocardiograms.
Outcome
Over 48 hours, the patient’s RV function improved, and an IVC filter was placed to reduce the risk of recurrent PE. He was subsequently discharged to the floor without requiring aggressive interventions.
This case highlights the importance of balancing intervention with the risk of complications.
FAQs About Pulmonary Embolism Management
1. What is the role of a perfusionist in managing PE?
Perfusionists manage cardiopulmonary bypass during surgical embolectomy and initiate/maintain ECMO support in refractory cases.
2. When should ECMO be considered in PE management?
ECMO is indicated in cases of hemodynamic collapse, refractory PE, or when patients cannot tolerate thrombolysis due to bleeding risk.
3. What are the risks of catheter-directed thrombolysis (CDT)?
CDT carries a lower risk of bleeding compared to systemic thrombolysis but may cause access-site bleeding or clot fragmentation.
4. How does a PERT team improve outcomes?
PERT teams streamline decision-making by bringing together specialists from multiple disciplines, ensuring timely and appropriate interventions.
5. What are the contraindications to thrombolysis?
Absolute contraindications include active bleeding, recent intracranial hemorrhage, or major surgery within the past 10 days.
6. What is the difference between VA and VV ECMO?
VA ECMO provides both cardiac and respiratory support, while VV ECMO primarily supports oxygenation.
7. Can surgical embolectomy be performed in patients with recent trauma?
Yes, but it requires careful evaluation of bleeding risk and clot location. Collaboration with perfusionists is essential for managing bypass.
8. What imaging studies are used to diagnose PE?
CT pulmonary angiography is the gold standard, but echocardiography and D-dimer testing are also valuable.
9. What is the role of an IVC filter in PE management?
IVC filters prevent recurrent PE in patients with contraindications to anticoagulation or those who develop PE despite therapeutic anticoagulation.
10. How can RV dysfunction be monitored in PE patients?
Serial echocardiograms, biomarkers like troponin and BNP, and clinical assessment are used to monitor RV function.
Why Choose CardiPerf.com ?
At CardiPerf.com , we are committed to providing healthcare professionals with the tools and knowledge they need to excel in cardiovascular care. Whether you’re a perfusionist, cardiac surgeon, intensivist, cardiac anesthesiologist, or cardiologist, our resources are designed to support your practice.
Explore our:
- Webinars : Learn from leading experts.
- Guidelines : Access evidence-based protocols for multidisciplinary care.
- Tools : Download checklists and templates.
Call to Action
Ready to take your PE management skills to the next level? Visit CardiPerf.com today to access exclusive resources, expert insights, and actionable tools tailored to your specialty. Together, we can improve outcomes for patients with pulmonary embolism.