Perioperative cardiac arrest during the induction of anesthesia is a rare but life-threatening event that poses a serious challenge to healthcare providers in cardiac surgery. When it occurs, quick diagnosis, decisive action, and seamless teamwork are critical for patient survival. This article explores the causes of perioperative cardiac arrest, outlines the roles of various healthcare providers, provides insights into managing such emergencies during cardiac surgery, and includes a case scenario to demonstrate the real-world application of these concepts.
What is Perioperative Cardiac Arrest?
Perioperative cardiac arrest refers to a sudden cessation of cardiac activity during the perioperative period, including anesthesia induction. It is a medical emergency that requires immediate attention from a well-coordinated team of anesthesiologists, surgeons, perfusionists, nurses, and other healthcare professionals. While rare, understanding the causes, diagnosis, and management strategies is essential for improving outcomes.
Causes of Cardiac Arrest During Anesthesia Induction
Perioperative cardiac arrest during anesthesia induction can be triggered by a variety of factors. Some of the most common causes include:

1. Hypoxia and Hypercarbia
- Respiratory depression caused by anesthesia agents such as propofol can lead to inadequate oxygenation, resulting in hypoxia and hypercarbia, both of which can precipitate cardiac arrest.
2. Medication-Related Events
- Anesthetic agents, opioids, and muscle relaxants can induce profound hypotension or bradycardia. In patients with preexisting cardiovascular conditions, the effects of these drugs can be amplified, increasing the risk of cardiac arrest.
3. Pre-existing Cardiovascular Conditions
- Patients with coronary artery disease, valvular heart disease, or a history of arrhythmias are at higher risk of cardiac arrest during anesthesia induction, as they may have an exaggerated response to anesthetic agents.
4. Electrolyte Imbalances
- Potassium or calcium imbalances, often found in patients with chronic diseases or renal failure, can increase the risk of arrhythmias, leading to cardiac arrest.
5. Anaphylaxis
- Although rare, an allergic reaction to anesthetic agents or muscle relaxants can cause anaphylactic shock, leading to sudden cardiovascular collapse.
6. Autonomic Nervous System Responses
- A vagal response, particularly in patients with heart disease, may lead to severe bradycardia or even cardiac arrest during anesthesia induction.
7. Mechanical Causes
- Conditions like cardiac tamponade or tension pneumothorax can be aggravated during induction, leading to sudden hemodynamic collapse.
Managing Cardiac Arrest During Anesthesia Induction: The Team’s Role
When a cardiac arrest occurs, the response must be swift and coordinated. Each member of the healthcare team has a specific role to play in managing the situation.
1. The Anesthesiologist
- The anesthesiologist is responsible for airway management, ventilation, and the administration of medications. They must rapidly identify the cause of the cardiac arrest, whether it’s related to drug overdose, anaphylaxis, or an underlying cardiovascular condition, and take appropriate action such as administering epinephrine or reversing medications.
2. The Surgeon
- The cardiac surgeon is often involved if the cause of the arrest is mechanical, such as cardiac tamponade or tension pneumothorax. In such cases, immediate surgical intervention may be necessary to correct the problem.
3. The Cardiologist
- If available, the cardiologist assists in evaluating the patient’s cardiac condition, especially if underlying coronary artery disease or other structural issues may have contributed to the arrest.
4. The Perfusionist
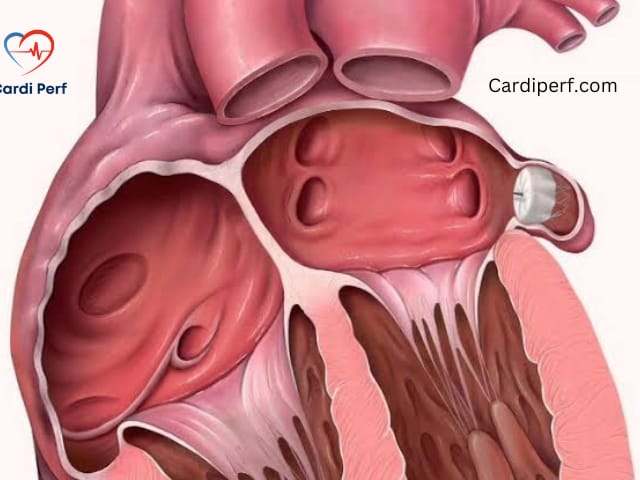
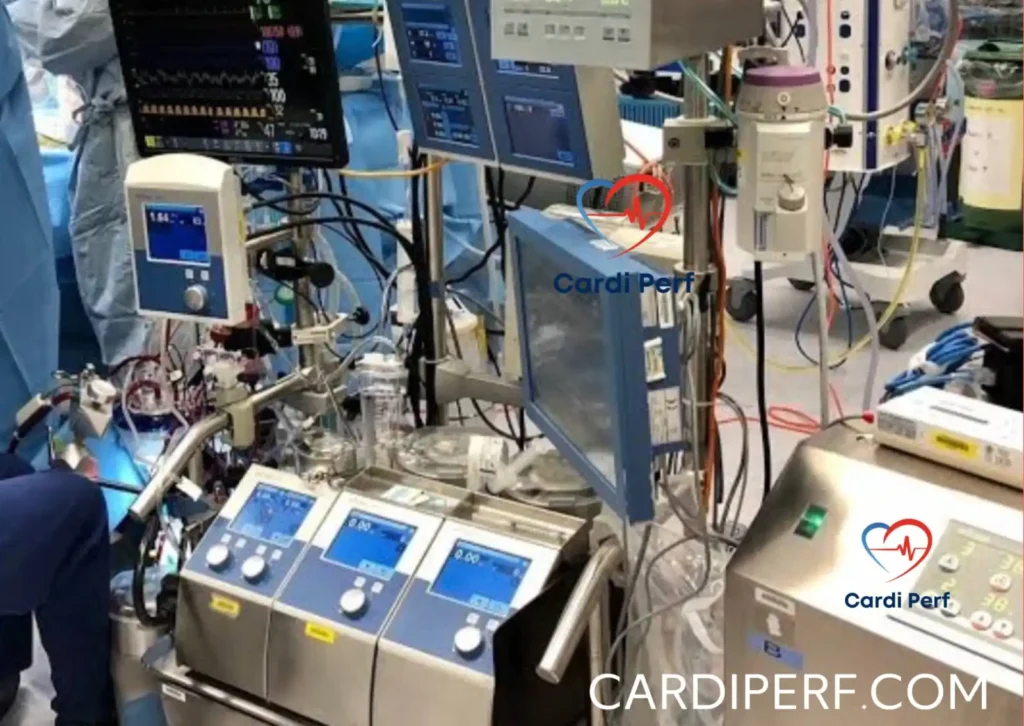
- Key Role in Circulatory Support: The perfusionist is essential in managing a cardiac arrest, particularly in cases requiring advanced circulatory support. In the event of prolonged cardiac arrest, the perfusionist will initiate cardiopulmonary bypass using the heart-lung machine. This allows the heart to rest and heal while maintaining oxygenation and circulation.
- ECMO Setup: In cases where cardiopulmonary bypass is not sufficient, the perfusionist may quickly prepare and initiate extracorporeal membrane oxygenation (ECMO). ECMO provides temporary mechanical circulatory support when the heart and/or lungs cannot function adequately, allowing the surgical team to focus on diagnosing and treating the underlying cause of the arrest.
- Blood Gas and Hemodynamic Monitoring: The perfusionist is responsible for continuously monitoring the patient’s hemodynamics and blood gases during bypass. This is critical for managing oxygenation and acid-base balance, ensuring the patient is stable while awaiting corrective treatment.
- Coordination with the Team: The perfusionist works closely with the anesthesiologist, surgeon, and other team members to ensure optimal perfusion pressures, oxygenation, and acid-base status during the emergency. Their timely intervention can make a significant difference in the patient’s outcome.
5. The Operating Room Nurse
- The operating room nurse ensures that all emergency drugs and equipment are available and ready. They also assist the anesthesiologist and surgeon by coordinating the team and supporting resuscitation efforts.
6. The EKG Technician
- Continuous ECG monitoring is crucial during perioperative cardiac arrest. The EKG technician helps interpret rhythm disturbances, enabling the team to make decisions about whether defibrillation or other interventions are needed.
Immediate Actions During Perioperative Cardiac Arrest
The first few minutes following a cardiac arrest are crucial. Here are the key actions that healthcare providers should take:
- Ensure Adequate Oxygenation and Ventilation:
- Airway management is the first priority. If the patient is not breathing, initiate bag-mask ventilation or intubate to secure the airway. Supplemental oxygen should be administered immediately.
- Initiate Cardiopulmonary Resuscitation (CPR):
- If the patient is in cardiac arrest, high-quality chest compressions should begin immediately. This provides blood flow to vital organs and buys time for further interventions.
- Follow Advanced Cardiac Life Support (ACLS) Protocols:
- Medications such as epinephrine and atropine should be administered as per ACLS guidelines. Defibrillation may be required for arrhythmias like ventricular fibrillation.
- Rapid Diagnostic Assessment:
- Point-of-care blood testing (e.g., ABGs, lactate, electrolytes) can provide valuable information on potential causes like metabolic acidosis or electrolyte disturbances.
- Intraoperative Circulatory Support:
- If the patient remains unstable, intra-aortic balloon pump (IABP) or ECMO can provide circulatory support and stabilize the patient long enough for corrective measures to be implemented.
Case Scenario: Perioperative Cardiac Arrest During Anesthesia Induction
Patient Background:
A 65-year-old male with a history of coronary artery disease, diabetes, and hypertension is scheduled for elective coronary artery bypass grafting (CABG). His preoperative assessments show mild left ventricular dysfunction (ejection fraction of 40%). He is taking beta-blockers, aspirin, and statins. The patient is NPO for 8 hours prior to surgery, and baseline vital signs are stable.
Induction of Anesthesia:
The anesthesia team prepares for induction with propofol, fentanyl, and rocuronium. The patient is given the induction dose of propofol, but moments after administration, he begins to show signs of bradycardia (heart rate drops to 35 bpm), followed by a sudden drop in blood pressure (systolic BP of 60 mmHg). The anesthesiologist attempts to reverse the bradycardia with atropine and administers phenylephrine to increase the blood pressure.
However, the patient’s condition deteriorates, and his heart rate drops further, eventually leading to cardiac arrest. Immediate chest compressions are initiated.
Team Response:
- Perfusionist Role:
- The perfusionist quickly sets up the heart-lung machine for cardiopulmonary bypass. Since the arrest is refractory to medications and defibrillation, the heart-lung machine is initiated, providing adequate oxygenation and circulation while the surgical team works to identify and treat the underlying cause.
- Anesthesiologist Role:
- The anesthesiologist manages the airway, continuing ventilation, and reassesses the pharmacological interventions. Epinephrine is administered, and an ECG monitor reveals asystole, indicating that the heart is not responding to resuscitation efforts.
- Surgeon Role:
- The surgeon prepares for a potential intraoperative intervention, considering the possibility of cardiac tamponade or other mechanical causes. In this case, the surgeon begins evaluating the patient’s chest for signs of pericardial effusion.
- EKG Technician:
- Continuous ECG monitoring helps confirm the rhythms and guides the decision-making process for further treatment.
Outcome:
After 20 minutes of successful ECMO support and ongoing resuscitation, the patient is stabilized. The cause of the arrest was identified as bradycardia due to high-dose propofol in combination with preexisting heart disease. The patient is transferred to the ICU for post-resuscitation care, including neurological assessment, and later undergoes CABG successfully.
Post-Resuscitation Care
After stabilizing the patient, it’s critical to focus on the following:
- Neurological Assessment:
- Early neurological assessments should be performed to detect any signs of brain injury, especially if the arrest was prolonged.
- Temperature Management:
- Therapeutic hypothermia may be used to protect the brain and organs from ischemic damage.
- Ongoing Monitoring:
- Continuous monitoring for signs of organ failure, especially renal and hepatic function, is crucial in the post-resuscitation phase.
- Re-evaluation of Underlying Causes:
- A thorough evaluation of the patient’s cardiovascular status should be conducted to determine if further interventions or monitoring are needed.
FAQs for Healthcare Providers
Q1: What are the common causes of cardiac arrest during anesthesia induction?
- The causes can include hypoxia, medication effects, underlying cardiovascular disease, electrolyte imbalances, anaphylaxis, and autonomic responses.
Q2: How can healthcare providers quickly identify the cause of cardiac arrest?
- Through airway management, continuous ECG monitoring, physical examination, and point-of-care lab tests such as blood gases and electrolytes.
Q3: What role does the perfusionist play during a perioperative cardiac arrest?
- The perfusionist is crucial in providing circulatory support via cardiopulmonary bypass or ECMO, monitoring blood gases, and working with the team to stabilize the patient.
Q4: When should ECMO or IABP be considered?
- If the arrest is prolonged or there is severe myocardial dysfunction, ECMO or IABP can provide critical circulatory support.
Q5: What medications should be considered during resuscitation?
- Epinephrine, atropine, vasopressors, and antiarrhythmic drugs like amiodarone or lidocaine may be used.
Q6: What is the role of the anesthesia provider during a perioperative cardiac arrest?
- The anesthesiologist manages the airway, initiates ACLS, and ensures proper drug administration to stabilize the patient.
Conclusion
While perioperative cardiac arrest during induction is rare, it demands swift action and precise coordination from the entire team. Understanding the causes and roles of each team member can significantly improve patient outcomes and ensure the best possible care during a cardiac crisis. In cardiac surgery, preparation, teamwork, and prompt decision-making are paramount in navigating such critical situations. for update information visit us at cardiperf.com