A cardiovascular perfusionist is responsible for a variety of important roles during heart surgeries and many complex medical procedures. These highly trained professionals are the ones running the heart-lung machine. This device assumes the life-supporting functions of the heart and lungs while the surgery is performed.
By controlling blood flow and oxygenation, they keep the patient’s body alive and able to function normally. Their work demands great precision, attention to detail, and a thorough understanding of human physiology, medical devices, and surgical protocols.
CV perfusionists work side by side with surgeons, anesthesiologists, and other members of the medical team to ensure continuous, effective support is delivered during surgery. Their profound expertise directly impacts patient outcomes and makes them a vital member of the healthcare team.
By knowing their unique role, you can begin to appreciate the complexities that today’s modern medicine and surgical care have created.
Key Takeaways
- CV perfusionists are specialized, highly trained, healthcare professionals. During extensive cardiac surgeries they are tasked with completely taking over the circulatory and respiratory systems, running complex heart-lung machines, and managing critical medications.
- They prime intricate medical devices and monitor patient vitals on an ongoing basis. They partner with surgeons and anesthesiologists to maintain stability and safety during the course of procedures.
- To be a perfusionist, you need to undergo a rigorous academic experience. This involves receiving a four-year degree in the sciences, completing an accredited perfusion program, and passing the American Board of Cardiovascular Perfusion certification exam.
- To thrive in this new role, you will require deep technical expertise in perfusion technology. Strong interpersonal skills are necessary for collaboration, as well as critical thinking skills to address complex, real-time, high-stakes challenges.
- Perfusionists are an integral members of the surgical team, despite their non-MD status. They work intimately with cardiothoracic physicians to achieve the best results in the most complicated cardiac procedures.
- The workplace is very exciting and fast-paced. This includes working long hours in operating rooms and intensive care units that require flexibility, determination and an unwavering focus on maintaining a clean and orderly environment.
What Is a Cardiovascular Perfusionist

1. Definition of the role
A cardiovascular perfusionist is a highly trained healthcare professional. They are responsible for maintaining the circulatory and respiratory functions during complicated surgical procedures, particularly in cardiac surgeries.
Their main role is to run the CPB (cardiopulmonary bypass) on Heart Lung Machine machine. This machine serves as an artificial heart and lung, taking over all functions of both organs temporarily. This machine is responsible for making sure oxygenated blood continues to flow through the patient’s body.
It enables surgeons to operate on a still heart without putting other vital organs in jeopardy. To perform this role effectively, perfusionists need to have a thorough knowledge of the respiratory system and the circulatory system.
This understanding enables them to control blood circulations and keep blood at perfect temp. They are capable of performing complex blood chemistry, including gases and some electrolytes, in real time during the procedure.
Their expertise is essential in keeping patients stable, which makes them absolutely vital during life-saving surgeries.
2. Key responsibilities in surgeries
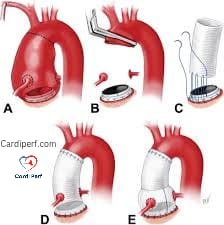
In preparation for surgery, perfusionists thoroughly test and prepare the CPB equipment to maintain perfect functionality. They choose the right cannulas for the procedure and do autologous blood collection when a transfusion might be needed.
During surgery, their tasks include operating the heart-lung machine, monitoring blood flow, and adjusting settings to meet the patient’s physiological needs. During a surgical procedure they are in constant control of pharmacological interventions by administering cardioprotective drugs.
Simultaneously, they work with surgeons and anesthesiologists to address any issues that come up during the procedure. If necessary, they might use an intra-aortic balloon pump to help circulate blood.
3. Importance in healthcare teams
Perfusionists are vital members of surgical teams, operating in concert with surgeons, anesthesiologists, and nurses. Their ability to adapt to the dynamic demands of the operating room directly impacts patient outcomes, particularly during intricate cardiac procedures.
So clear, competent teamwork and communication are critical. Perfusionists need to coordinate the biggest team in healthcare, working alongside surgeons and other medical professionals to keep surgery as seamless as possible.
Their mastery enhances the technical dimensions of surgery. It’s just as important in improving patient safety and recovery.
Educational Requirements for Cardiovascular Perfusionists
1. Academic qualifications needed
If you want to become a cardiovascular perfusionist, having a solid academic background especially in the sciences is crucial. Usually, this route starts with a bachelor’s degree in a related area, like biology, chemistry, or physics. Aspiring perfusionists are required to take 60-80 credit hours of pre-professional coursework.
They must develop a solid foundation in biology, anatomy, physiology, and chemistry. These didactic courses set the foundation for a perfusionist’s ability to understand and interpret complicated physiological processes. You’ll explore the intricacies of blood flow dynamics and advanced oxygenation techniques.
For example, knowledge of human anatomy is key in using extracorporeal machines during cardiac surgeries. Degrees and other educational experiences are only acceptable if completed through accredited programs, ensuring students have the requisite education to meet the high clinical standards of competence.
2. Certification and licensing process
Certification as a clinical perfusionist is a challenging process overseen by the American Board of Cardiovascular Perfusion (ABCP). Candidates are required to graduate from an accredited perfusion program and complete an established minimum number of clinical cases that show they have practical expertise.
Upon passing the certification exam, cardiovascular perfusionists must participate in yearly recertification. This rigorous process includes an ongoing requirement that they accumulate continuing education credits and verify their work experience.
This continuing education process makes sure that perfusionists are aware of the latest medical advancements, helping them to be experts in the clinical setting.
3. Specialized training programs
Specialized training programs are instrumental in developing the next generation of perfusionists. These programs, available at 18-19 U.S. Schools, consist of certificate, bachelor’s, and master’s degrees.
Institutions such as the Cleveland Clinic School of Cardiovascular Perfusion provide direct, hands-on, clinical education. After all, this critical hands-on experience is crucial for learning the intricate perfusion technologies.
Accredited by agencies including the Ohio State Board of Education, these programs equally prepare students to take state certification exams. For international students, graduating from a U.S.-based or Canadian program is a requirement for certification eligibility.
Skills Needed for Cardiovascular Perfusionists
1. Technical expertise required
To be a cardiovascular perfusionist, understanding medical technology is an integral part of the profession. Running a heart-lung machine requires absolute accuracy. Yet it requires a deep knowledge of its mechanics to successfully commandeer the heart and lungs during an operation.
Continuous patient monitoring of blood pressure, blood oxygen levels, heart rate, and more will go a long way to helping you know that everything on the machine is operating as it should. Well, you have all this expertise in hemodynamics—the study of blood flow through the circulatory system.
You perform blood gas analysis, determining the concentrations of oxygen and carbon dioxide in the blood, as well as blood pH levels. You need to have expertise in a range of perfusion technologies. This includes intra-aortic balloon pumps and ECMO (Extracorporeal Membrane Oxygenation) systems that are essential for supporting our most critically ill patients.
These skills are not a nice-to-have—they are mission critical to the patient’s survival.
2. Communication and teamwork skills
In the operating room, teamwork is not only a nice thing to have, it’s absolutely essential. When your role is even defined as a perfusionist, you serve as a connector between the surgical team, the anesthesiologists, and nursing staff, bringing everyone into harmony.
When things get busy, clear, concise communication prevents misinterpretation, which is critical during complex procedures. Let’s say a surgeon is performing a complex surgery on a 280 lb. Patient. Effective teamwork involves more than just coordinating technical tasks; it creates a climate in which each team member knows they have the support of their team.
Interpersonal skills go a long way in diffusing potential stressful situations. They help to establish trust within the team, which is so important in those high-stakes moments.
3. Problem-solving under pressure
Surgeries that require access to the heart are, by nature, high-pressure scenarios. Things you can’t foresee, such as sudden changes in a patient’s blood pressure or an equipment failure, can happen at any time.
As a perfusionist, you will need to be prepared to address these complications on the fly and find solutions expediently. Staying calm isn’t just a personal trait—it’s a professional requirement. Your ability to break down the issue and think critically will be most important.
They can make a possible catastrophe go off without a hitch. When you are using a heart-lung machine and it fails, you need to react right away. Everything you do has to be done with the intent of stabilizing the patient.
This is a heavy responsibility, one that requires a quick mind and a steady hand, particularly when lives are at stake.
Is a Cardiovascular Perfusionist a Doctor
1. Differences in roles and education
Cardiovascular perfusionists and medical doctors perform two very different roles inside the operating room. Each of these healthcare professionals brings their own unique expertise to the healthcare team. A cardiovascular perfusionist is the specialized practitioner who manages the cardiopulmonary bypass machine, among other things.
This machine, during open-heart surgeries, takes over the function of the heart and lungs. Aside from the logistical details of the surgery, their main concern is providing circulatory and respiratory support while keeping the patient’s blood flow and oxygen levels stable. By comparison, medical doctors, especially cardiothoracic surgeons, are the ones who are doing the actual surgical procedures and making the complex medical decisions during the surgery.
The educational pathways for these professions are worlds apart as well. If you want to become a certified cardiovascular perfusionist, that’s at least six years of education. This means completing a bachelor’s degree and then two years in an accredited perfusionist program.
Candidates are required to have completed at least 75 assisted procedures. They must pass the board exams administered by the American Board of Cardiovascular Perfusion (ABCP). As you all know, physicians have a very long training path. They undergo four years of medical school, often followed by three to eight years of residency training and sometimes further fellowships for subspecialty training.
Where doctors provide diagnostic insight and surgical skill, perfusionists provide technical expertise with life-support machinery. These unique skills help to round out the surgical team, which ensures that the team is multidisciplinary and focused on patient safety and successful outcomes.
2. Collaborative relationship in surgeries
The cardiac OR is an exciting place. Cardiovascular perfusionists and physicians work hand-in-hand to make sure that surgical procedures go as seamlessly as possible. Perfusionists are essential members of the cardiac surgery team, keeping a patient’s blood flowing and oxygenated through the cardiac bypass machine, often managing this process with little direct guidance.
On a coronary artery bypass graft (CABG), the surgeon’s full attention is on repairing the blocked arteries. In the background, the perfusionist or heart-lung machine operator professionally monitors and directs blood flow. By working together as a team, the surgical and physiological needs of the patient can be better addressed.
Mutual respect is key to this very collaborative environment. Each professional knows how serious the other’s role is, creating a collaborative atmosphere. The surgeon will call out blood pressure or oxygenation needs.
In turn, the perfusionist continually monitors and makes immediate and exact corrections to requirements. This high degree of coordination takes, in addition to technical expertise, clear communication and trust.
Collaboration significantly enhances decision-making, especially during complex cases. For example, if unexpected complications arise, the team can quickly evaluate options and adjust strategies.
This synergy between perfusionists and doctors underscores the importance of their partnership in achieving optimal patient outcomes.
Work Environment of Cardiovascular Perfusionists
1. Common Workplaces and Settings
Perfusionists mainly work in a hospital or large surgical center, and they are a vital member of the cardiovascular surgical team. Almost 90% of their time is spent within ORs that are managing cardiac cases. Perfusionists are not limited to the operating room.
You’ll see them in the cardiovascular intensive care unit (CVICU) and catheterization labs, where they provide immediate, critical cardiovascular support procedures. These highly educated professionals work in shifts to provide 24/7 coverage in these often very busy facilities. Therefore, their schedules typically include nights, weekends, and holidays.
Their responsibilities change from scenario to scenario, from scheduled, elective operations to intense, emergent life-saving procedures. For example, during emergency surgeries, they must quickly adapt to rapidly changing conditions, making critical decisions under stress.
Perfusionists at these specialized cardiac centers deal with more complex cases like heart transplants or pediatric cardiac surgeries. This versatility underscores the importance of being prepared to adapt and respond to a variety of clinical environments and patient populations.
2. Typical Daily Tasks and Duties
Perfusionists have a long day that begins with meticulous planning. They carefully calibrate and test devices such as heart-lung machines and heart monitors to make sure they operate flawlessly during surgery.
During surgeries, perfusionists keep a close eye on the patient’s vital signs and blood supply and oxygenation, maintaining homeostasis and stability all the way through the procedure. In other instances, they will draw and prepare the patient’s own blood for autologous transfusions.
Keeping detailed and precise records is an important part of their jobs. They record detailed data on procedures, equipment usage, and patient responses, which is essential for post-operative care and legal compliance.
Being open to continuous learning is key. By remaining abreast of industry innovations and techniques, they can make a meaningful, direct impact on performance in the field.
Challenges Faced by Cardiovascular Perfusionists
1. High-pressure situations in surgeries
The operating room is a highly stressful environment, particularly for cardiovascular perfusionists. They are responsible for operating the heart-lung machine, which takes over the functions of the heart and lungs during procedures like open heart surgery. When unexpected complications arise, such as a sudden drop in blood pressure or oxygen levels, the clinical perfusionist must adjust the machine settings immediately to ensure proper cardiopulmonary function.
These decisions are typically made in seconds and may have a direct effect on the patient’s survival. The intense, fast-moving environment of a surgical team demands in-the-moment communication and coordination in a high-stress, life-or-death scenario. The role is more than just technical skills, it’s about understanding the urgency of each action and still being able to think clearly and remain composed.
The weight of these high-stakes scenarios is what makes being a clinical perfusionist so profound, as they play a vital role in the success of heart operations and the overall health of patients.
2. Physical and mental demands of the role
These cardiovascular perfusionist professionals frequently experience long physically intense shifts. Or, they could be on their feet for several hours while monitoring intricate equipment in surgical suites requiring extreme concentration. Take, for instance, a complicated cardiac surgery, which can be eight or more hours long, with constant focus necessary to ensure the heart-lung machine is functioning properly.
The mental toll is just as big, though, with even the smallest lapse in focus potentially resulting in catastrophic impacts. Outside of the operating room, self-care is extremely important. They balance their work with performing stress, productive stress management, exercise and connection with their support systems to replenish their work.
This resilience is key to coping with their high-stress, highly technical workplace.
Conclusion
A career as a cardiovascular perfusionist is truly a rewarding health care career. You collaborate with surgical teams, control life-saving equipment, and have a direct, tangible impact on patients’ lives every day. The role requires intense technical skill, concentration, and a rigorous education, but the reward is immeasurable. You earn the chance to expand your knowledge base and tackle new, exhilarating obstacles in a dynamic and quickly evolving atmosphere.
If you care deeply about health care and perform well in high pressure situations, this may be the perfect career for you. Find your program, meet the medical professionals who work in this field and get started on your education today. A career as a cardiovascular perfusionist is a highly rewarding experience. Then you can go on to win a role in which every decision counts and no two days are the same. Your adventure begins on day one.
Frequently Asked Questions
What does a cardiovascular perfusionist do?
A cardiovascular perfusionist operates the heart-lung machine during critical heart operations, ensuring proper blood circulation and oxygenation when the patient’s heart is temporarily stopped. Their expertise in clinical perfusion is indispensable in high-stakes procedures like open-heart surgery.
What education is required to become a cardiovascular perfusionist?
To become a cardiovascular perfusionist, you begin with a bachelor’s degree and then complete a clinical perfusion education program, as certification is mandated in nearly every state.
Is a cardiovascular perfusionist a doctor?
A cardiovascular perfusionist is a highly trained medical professional who plays a vital role in heart operations.
What skills are important for cardiovascular perfusionists?
A few of those skills, such as advanced technical knowledge and excellent communication skills, are vital for clinical perfusionists to maintain patient safety while conducting heart operations under pressure.
Where do cardiovascular perfusionists work?
Cardiovascular perfusionists, vital members of the OR teams, typically work in hospitals or surgical centers, performing complex heart operations and vascular surgeries.
What challenges do cardiovascular perfusionists face?
The job can be rewarding, but it’s a high-stakes, stressful environment with serious pressures. Long hours and being on-call may take their toll on clinical perfusionists involved in critical care.
How much does a cardiovascular perfusionist typically earn?
The average annual salary for a clinical perfusionist varies based on location and years of experience, with most earning between $100,000 and $150,000 a year in the US, reflecting the importance of cardiovascular perfusion in heart operations.