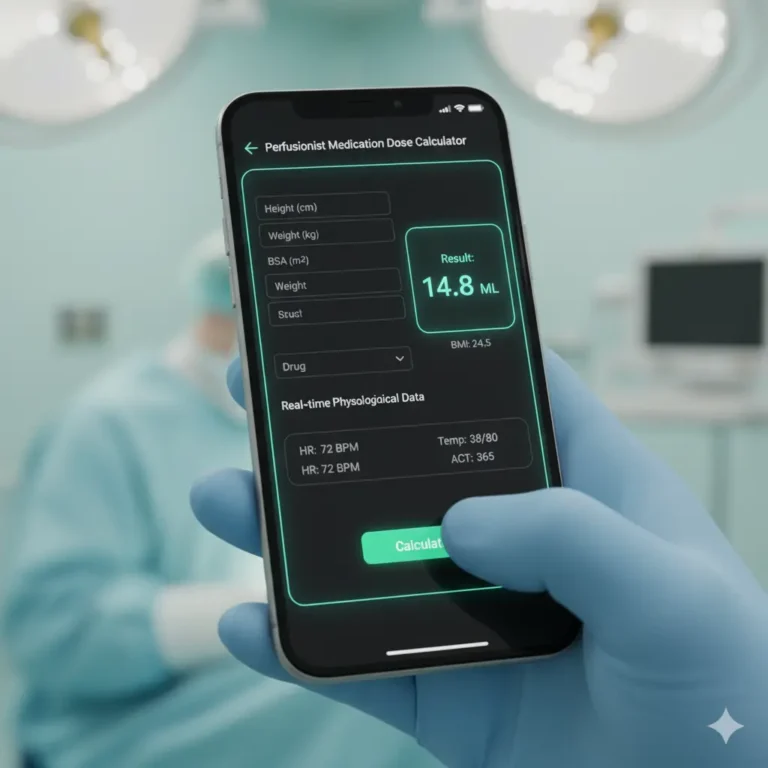
Sodium Bicarbonate Calculator
Sodium bicarbonate (NaHCO₃), a key alkalizing agent, plays a critical role in critical care, extracorporeal circulation, and anesthesia. Its ability to buffer acidosis makes it invaluable in managing metabolic acidosis, cardiopulmonary bypass (CPB), and intraoperative emergencies. However, its misuse can lead to complications like alkalosis or hypernatremia, posing risks in high-stakes environments.
This article provides a comprehensive guide on the safe use of sodium bicarbonate for perfusionists, critical care teams, and anesthesiologists. Focusing on evidence-based protocols, we address indications, dosing, risks, and practical considerations to optimize patient outcomes in acute care settings. With a deep dive into clinical applications and safety, this resource ensures professionals can leverage NaHCO₃ effectively while minimizing adverse effects.
Understanding Sodium Bicarbonate in Clinical Practice
Pharmacological Properties
Sodium bicarbonate is a systemic alkalizing agent that dissociates into sodium (Na⁺) and bicarbonate (HCO₃⁻) ions, buffering excess hydrogen ions to raise blood pH. Its rapid onset makes it ideal for acute metabolic acidosis, with effects visible within minutes when administered intravenously. Each 1 mEq/mL solution (e.g., 8.4% NaHCO₃) delivers 1 mmol/L of sodium and bicarbonate, requiring careful monitoring to avoid electrolyte imbalances.
Mechanism in Acid-Base Balance
In acidosis, NaHCO₃ neutralizes hydrogen ions, forming water and carbon dioxide (CO₂), which is exhaled via ventilation. This process corrects pH but increases CO₂, necessitating adequate ventilatory support. In CPB, it counters acid accumulation from hypoperfusion or hemodilution, maintaining physiological stability (StatPearls – Sodium Bicarbonate).
Why Safety is Paramount
The safe use of sodium bicarbonate is critical in critical care due to its narrow therapeutic window. Overcorrection can cause metabolic alkalosis, hypernatremia, or hypokalemia, while underdosing may fail to resolve acidosis. Perfusionists and anesthesiologists must balance its benefits with risks, especially in patients with compromised renal or cardiac function.
Clinical Indications for Sodium Bicarbonate
Metabolic Acidosis Management
Sodium bicarbonate is indicated for severe metabolic acidosis (pH < 7.2, HCO₃⁻ < 15 mmol/L) due to lactic acidosis, diabetic ketoacidosis (DKA), or renal failure. It restores pH to improve myocardial contractility and catecholamine responsiveness. In critical care, it’s often used when base deficit exceeds -10 mEq/L, guided by arterial blood gas (ABG) analysis (Medscape – Sodium Bicarbonate Dosing).
Cardiopulmonary Bypass (CPB)
Perfusionists rely on NaHCO₃ during CPB to counteract acidosis from hemodilution, hypothermia, or prolonged bypass times. It’s typically added to the prime solution or given as a bolus to maintain pH 7.35–7.45. The safe use of sodium bicarbonate in CPB involves titrating doses based on serial ABGs to avoid overcorrection.
Cardiac Arrest and Resuscitation
In cardiac arrest, NaHCO₃ may be considered for prolonged resuscitation (>10–15 minutes) with documented acidosis (pH < 7.2). However, routine use is discouraged due to risks of paradoxical intracellular acidosis from CO₂ accumulation ([American Heart Association Guidelines]). Anesthesiologists must weigh its use against ventilatory status.
Hyperkalemia and Drug Overdose
Sodium bicarbonate can temporize hyperkalemia by driving potassium into cells via alkalization, often combined with insulin-dextrose. It’s also used in overdoses of tricyclic antidepressants or salicylates to enhance urinary excretion by alkalizing urine (pH > 7.5). Precise dosing is critical to avoid complications.
Benefits of Sodium Bicarbonate in Critical Care
Rapid Correction of Acidosis
NaHCO₃ swiftly corrects severe acidosis, improving hemodynamic stability. In shock states, restoring pH enhances vasopressor efficacy, reducing catecholamine requirements. Studies show improved survival in sepsis-related acidosis when pH is normalized (WebMD – Sodium Bicarbonate).
Stabilization in CPB
During CPB, NaHCO₃ maintains acid-base homeostasis, reducing the risk of arrhythmias or organ dysfunction. Perfusionists note its role in countering lactic acid buildup, ensuring stable perfusion parameters ([Journal of Cardiothoracic Surgery]).
Adjunct in Toxicological Emergencies
In salicylate poisoning, NaHCO₃ facilitates urinary clearance, reducing toxicity. Similarly, in hyperkalemia, it provides a rapid bridge to definitive therapies like dialysis, critical in ICU settings.
Versatility Across Specialties
From anesthesia induction to ICU management, NaHCO₃’s broad utility makes it a staple. Its availability as an IV solution ensures immediate access in emergencies, enhancing its value in high-acuity care.
Risks and Complications of Sodium Bicarbonate
Metabolic Alkalosis
Overzealous administration can cause metabolic alkalosis (pH > 7.45), impairing oxygen delivery due to left-shifted oxyhemoglobin dissociation curves. This is particularly risky in ventilated patients with limited CO₂ clearance (Mayo Clinic – Sodium Bicarbonate).
Hypernatremia and Fluid Overload
Each 50 mL of 8.4% NaHCO₃ delivers 1,000 mg of sodium, risking hypernatremia or fluid overload in patients with heart failure or renal impairment. Critical care teams must monitor sodium levels, especially in prolonged infusions.
Hypokalemia and Hypocalcemia
Alkalization drives potassium and calcium intracellularly, potentially causing hypokalemia or hypocalcemia. This can trigger arrhythmias, particularly in cardiac surgery or ICU patients. The safe use of sodium bicarbonate requires concurrent electrolyte monitoring.
Paradoxical Intracellular Acidosis
Rapid CO₂ production from NaHCO₃ can worsen intracellular acidosis in poorly ventilated patients, as CO₂ diffuses into cells faster than bicarbonate. Anesthesiologists must ensure adequate minute ventilation before administration.
Guidelines for Safe Use of Sodium Bicarbonate
Dosing Protocols
- Metabolic Acidosis: Calculate dose using:
Dose (mEq) = Base Deficit × Weight (kg) × 0.3 (extracellular fluid volume). Administer half the dose over 5–10 minutes, reassess with ABG, and give the remainder if needed. Typical *Typical dose: 1–2 mEq/kg IV over 10–15 minutes (Medscape). - CPB: Add 50–100 mEq to prime or bolus 1–2 mEq/kg based on ABG.
- Hyperkalemia/Salicylate Overdose: 1–2 mEq/kg IV push, repeated every 15–30 minutes to achieve urine pH > 7.5.
- Cardiac Arrest: 1 mEq/kg IV, repeated every 10 minutes if indicated, per ACLS guidelines.
Administration Best Practices
- Dilution: Dilute 8.4% NaHCO₃ (1 mEq/mL) in D5W or sterile water for infusions to reduce osmolarity.
- Monitoring: Check ABG, electrolytes, and ECG every 15–30 minutes during therapy.
- Ventilation: Ensure adequate ventilation (PaCO₂ < 40 mmHg) to clear CO₂.
- Compatibility: Avoid mixing with calcium-containing solutions to prevent precipitation.
Perfusionist-Specific Tips
During CPB, monitor pH and base deficit every 15–30 minutes. Adjust NaHCO₃ in 25–50 mEq increments, avoiding bolus doses > 2 mEq/kg to prevent alkalosis. Coordinate with anesthesiologists for real-time ABG data.
Anesthesiologist and ICU Considerations
- Pre-Administration: Confirm indication (e.g., pH < 7.2, base deficit > 10).
- Post-Administration: Monitor for signs of alkalosis (e.g., carpopedal spasm, confusion) or hypernatremia (e.g., edema, hypertension).
- Documentation: Record dose, timing, and ABG results for continuity of care.
Contraindications and Precautions
Absolute Contraindications
- Metabolic Alkalosis: pH > 7.45 or HCO₃⁻ > 30 mmol/L.
- Hypoventilation: PaCO₂ > 45 mmHg without mechanical ventilation.
- Severe Pulmonary Edema: Due to sodium load.
- Hypocalcemia: Unless corrected, to avoid tetany (WebMD).
Relative Contraindications
- Heart Failure: Monitor for fluid overload.
- Renal Failure: Risk of sodium retention and alkalosis.
- Chronic Steroid Use: Increases alkalosis risk.
Special Populations
- Pediatrics: Use 4.2% NaHCO₃ (0.5 mEq/mL) to reduce osmolarity. Dose: 1–2 mEq/kg.
- Elderly: Lower doses (0.5–1 mEq/kg) due to reduced renal clearance.
- Pregnancy: Avoid unless critical, as sodium load may cause fetal edema.
FAQs for Critical Care Professionals
When Should NaHCO₃ Be Avoided in Cardiac Arrest?
Avoid routine use in the first 10 minutes of ACLS unless hyperkalemia or acidosis is confirmed. Prioritize ventilation and epinephrine per guidelines.
How Do I Manage Overcorrection?
If pH > 7.45, stop NaHCO₃, increase ventilation, and consider acetazolamide (250–500 mg IV) to excrete excess bicarbonate. Monitor electrolytes closely.
Can NaHCO₃ Be Used in DKA?
Use cautiously in DKA, only if pH < 6.9 and after insulin therapy, as it may worsen hypokalemia or delay ketoacid clearance (Medical News Today).
What’s the Role in ECMO?
In ECMO, NaHCO₃ corrects acidosis from circuit-related hemolysis or low flow. Dose based on ABG, typically 1 mEq/kg every 4–6 hours, with continuous monitoring.
Conclusion
The safe use of sodium bicarbonate in critical care, perfusion, and anesthesia demands precision, vigilance, and collaboration. Its ability to correct acidosis, stabilize CPB, and manage toxicological emergencies makes it indispensable, but risks like alkalosis, hypernatremia, and hypokalemia require careful management. Perfusionists must titrate doses based on real-time ABGs, anesthesiologists should ensure ventilatory support, and critical care teams need to monitor electrolytes and clinical status. By adhering to evidence-based protocols—such as calculated dosing, serial monitoring, and clear contraindications—professionals can optimize outcomes while minimizing complications. This guide equips you with the knowledge to use NaHCO₃ safely, ensuring patient safety in the most critical moments.
Sources: