The Intra-Aortic Balloon Pump (IABP) is a mechanical device used to support patients with heart failure or shock. It helps increase blood flow to the heart and other vital organs by reducing the workload of the heart. The device works by inflating a balloon in the descending aorta during diastole (the relaxation phase of the heart) and deflating it during systole (when the heart contracts). This cyclical action increases coronary perfusion and reduces afterload, thus improving cardiac output and oxygen delivery to the tissues.

Indications for IABP Therap
IABP therapy is not used for every heart patient; it is specifically designed for cases where the heart is under significant strain. The primary indications for IABP therapy include:
1. Cardiogenic Shock
Cardiogenic shock occurs when the heart can no longer pump enough blood to meet the body’s demands. This often results from a severe heart attack or heart failure. IABP therapy provides immediate circulatory support, giving the heart time to recover by reducing its workload and improving coronary artery blood flow.
2. Acute Myocardial Infarction (MI) with Severe Left Ventricular Dysfunction
In patients who experience a massive heart attack, the left ventricle (the heart’s main pumping chamber) may be severely compromised. IABP therapy can improve coronary blood flow, reducing the impact of the infarction and supporting heart function during the critical phase of recovery.
3. Post-Cardiotomy Cardiogenic Shock
After heart surgery, especially coronary artery bypass grafting (CABG) or valve repair, some patients may experience a drop in cardiac output, leading to cardiogenic shock. The IABP is used to support the heart while it recovers from surgery.
4. Bridge to Heart Transplantation
In patients awaiting a heart transplant, IABP can provide temporary support to the heart. This therapy can help manage symptoms of heart failure and improve survival rates while the patient awaits a suitable donor heart.
Contraindications for IABP Therapy
While IABP therapy is beneficial in many cases, it is not suitable for everyone. There are several contraindications that healthcare providers need to consider before placing an IABP.
1. Severe Aortic Regurgitation
Aortic regurgitation occurs when the aortic valve does not close properly, causing blood to flow back into the left ventricle. Inserting an IABP can worsen the regurgitation by increasing the volume of blood that leaks backward into the heart.
2. Aortic Aneurysm
Patients with an aortic aneurysm, a bulging or weakening of the aortic wall, should not undergo IABP therapy. The pressure exerted by the balloon can increase the risk of aneurysm rupture.
3. Severe Peripheral Vascular Disease
In patients with advanced peripheral vascular disease (PVD), inserting the IABP catheter into the femoral artery may be difficult or dangerous. The risk of developing limb ischemia (lack of blood flow to the legs) is heightened, and other options may need to be considered.
4. Active Bleeding
Since IABP therapy requires the use of anticoagulation (blood thinners) to prevent clot formation, it is contraindicated in patients with active bleeding or those at high risk of bleeding.
Step-by-Step Process for IABP Insertion
The insertion of an IABP catheter is a critical procedure that should be performed by a skilled medical team. Here’s an outline of the typical steps involved in IABP insertion:
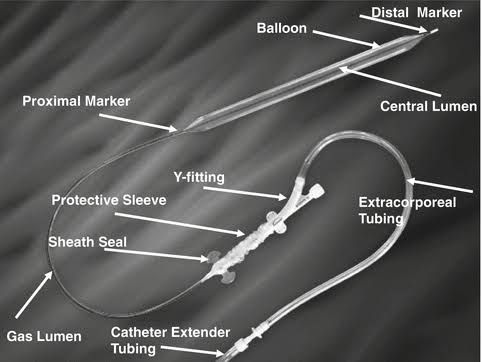
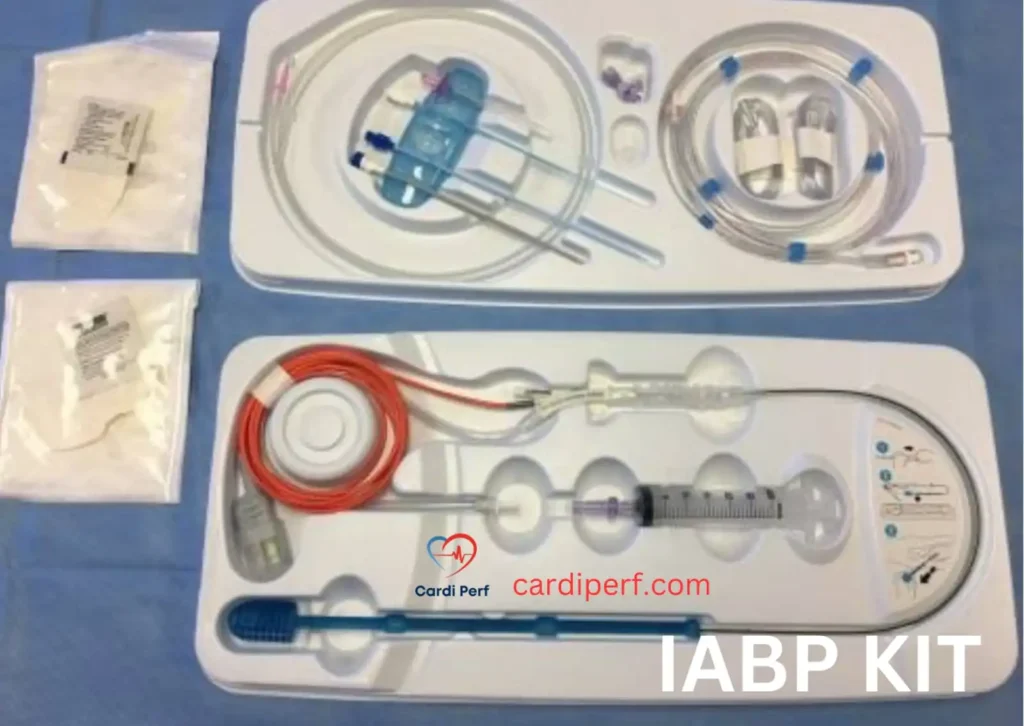
1. Catheter Selection and Preparation
The healthcare team Most Cardiologist , Cardiac Surgeon and Perfusionist will select the appropriate size and type of IABP catheter based on the patient’s anatomy and the specific needs of the case. The catheter is flushed with heparinized saline to remove air and ensure it is ready for insertion.
Heparin Therapy
To prevent thromboembolic complications during IABP therapy, heparin anticoagulation is crucial.
Heparin Administration Guidelines
To ensure effective anticoagulation, follow these guidelines:
- Initial dose: Administer an initial bolus dose of 2,000-5,000 units of heparin intravenously (IV) when IABP therapy is initiated.
- Continuous infusion: Start a continuous heparin infusion at a rate of 500-1,000 units/hour IV.
- Monitoring: Monitor activated partial thromboplastin time (aPTT) every 2-4 hours and adjust the heparin infusion rate accordingly.
- Target aPTT range: Maintain an aPTT range of 1.5-2.5 times the normal range (usually 50-70 seconds).
- Dose adjustments: Adjust the heparin infusion rate based on aPTT results:
- If aPTT is below the target range, increase the heparin infusion rate by 100-200 units/hour.
- If aPTT is above the target range, decrease the heparin infusion rate by 100-200 units/hour.
- Re-bolus: If aPTT falls below the target range, consider re-bolusing.
Activated Clotting Time (ACT) Monitoring
When using ACT instead of aPTT, target values vary depending on the clinical context and anticoagulant used:
- For unfractionated heparin (UFH) therapy: 150-200 seconds (or 120-180 seconds in some institutions)
- For high-risk patients (e.g., those with mechanical heart valves): 200-250 seconds
- For low molecular weight heparin (LMWH), ACT is not typically used for monitoring
Heparin-Induced Thrombocytopenia (HIT)
HIT is a serious complication of heparin therapy. Be aware of the symptoms:
- Decrease in platelet count (thrombocytopenia)
- Formation of blood clots (thrombosis) in arteries or veins
- Skin necrosis at the site of heparin injection
- Acute systemic reactions (e.g., fever, chills, hypertension)
Diagnose HIT using laboratory tests
(4Ts score, ELISA, and functional assays). Treat HIT by discontinuing heparin, initiating alternative anticoagulants, and monitoring platelet count and thrombotic complication
Conclusion
Heparin therapy is crucial in IABP patients to prevent thromboembolic complications. By following the guidelines outlined above and being aware of the risks of HIT, healthcare providers can ensure effective anticoagulation and optimal patient outcomes.
2. Insertion via
a) the Femoral Artery (Common)
The most common insertion site for the IABP catheter is the femoral artery, located in the groin. This site is preferred because it allows for easy access to the aorta, where the balloon needs to be placed. The catheter is inserted through the femoral artery using a guidewire and fluoroscopy (real-time X-ray) to ensure accurate placement.
Alternative Routes:
b) Axillary/Subclavian/Brachial Arteries:
These arteries in the upper body can be used as alternative access sites if femoral artery access is not feasible. This may be necessary in patients with severe peripheral vascular disease or aortic aneurysms.
3. Balloon Positioning
Once the catheter is in place, the balloon is carefully positioned in the descending aorta, approximately 2-3 cm below the left subclavian artery. This placement is crucial to ensure that the balloon inflates and deflates in synchrony with the cardiac cycle, providing optimal support for the heart.
How Does IABP Therapy Work?

IABP therapy works by inflating and deflating a balloon in the descending aorta during the cardiac cycle. The inflation occurs during diastole (the relaxation phase), which increases coronary blood flow to the heart muscle, allowing it to receive more oxygen and nutrients. The deflation occurs during systole (the contraction phase), which reduces the afterload, or the resistance the heart has to overcome to pump blood. This helps the heart pump more efficiently and improves overall cardiac output.
Monitoring IABP Therapy
During IABP therapy, it is critical to monitor the patient’s hemodynamic status to ensure the therapy is working as expected. Healthcare providers use specialized equipment Intra-Aortic Baloon Pumps (IABP) to monitor the following:
Pressure Waveforms:
These waveforms show the synchronization of balloon inflation and deflation with the patient’s cardiac cycle.
Balloon Function:
The inflation and deflation timing must be consistent with the patient’s heartbeat for optimal effectiveness.
Vital Signs:
Continuous monitoring of blood pressure, heart rate, and oxygen levels is essential to assess the patient’s response to therapy.
Complications and Emergencies in IABP Therapy
Although IABP therapy can save lives, it is not without its risks. There are several potential complications that healthcare providers need to be aware of:
1. Limb Ischemia
One of the most common complications of IABP therapy is limb ischemia, especially if the catheter is inserted through the femoral artery. This occurs when blood flow to the legs is restricted, potentially causing tissue damage. To manage this, healthcare providers monitor the affected limb closely for signs of poor circulation and adjust the catheter position if needed.
2. Balloon Rupture
In rare cases, the balloon may rupture, leading to a sudden loss of pressure and decreased blood flow. If a rupture occurs, the IABP should be immediately stopped, and the catheter should be removed. The patient may require immediate supportive measures, including medication and IABP replacement but in rare cases possibly surgery.
3. Bleeding and Vascular Complications
Since the IABP catheter is inserted through a large artery, bleeding can occur at the insertion site. This risk is further exacerbated if the patient is on anticoagulation therapy. In the event of bleeding, pressure should be applied to the insertion site, and further interventions, such as transfusions or surgical repair in rare case, may be necessary.
4. Infection
Infection is another risk, particularly in patients who need prolonged IABP therapy. Proper sterile technique during catheter insertion and diligent care of the insertion site can help reduce the risk of infection.
Training and Education for Healthcare Providers
Given the complexity of IABP therapy, it is essential for healthcare providers to receive thorough training in both the technical aspects of the device and the management of potential complications. Training should include:
Device Operation

Intra-Aortic Balloon Pump (IABP) Malfunction, their rectification strategies, and possible outcomes:
Here are different scenarios of Intra-Aortic Balloon Pump (IABP) Malfunction, their rectification strategies, and possible outcomes:
Scenario 1: IABP Balloon Rupture
Problem:
A 68-year-old male with cardiogenic shock post-myocardial infarction is on IABP support. The ICU team notices blood in the helium line, indicating balloon rupture. The console also shows a low helium pressure alarm.
Rectification:
- Immediate Actions:
- Stop the IABP and place the patient on vasopressor support (if needed).
- Do NOT attempt to reinflate the balloon to prevent thrombus formation.
- Balloon Removal Approach:
- If recognized early (<60 minutes):
- Pass a guidewire through the central lumen.
- Withdraw the ruptured balloon and pass a new balloon over the wire.
- If >60 minutes or resistance encountered:
- Prepare for surgical removal via femoral cutdown.
- If recognized early (<60 minutes):
- Monitor for Complications:
- Assess for limb ischemia, cholesterol embolization, or retroperitoneal bleeding.
Outcome:
- If managed promptly, balloon replacement is successful with no adverse effects.
- Delayed recognition may lead to arterial occlusion, requiring embolectomy or bypass surgery.
Scenario 2: IABP Entrapment (Cannot Be Withdrawn)
Problem:
A 72-year-old post-CABG patient requires IABP weaning. Upon attempting removal, the balloon is stuck in the sheath. The patient now has cold extremities and worsening leg ischemia.
Rectification:
- Confirm Diagnosis:
- Check balloon position via fluoroscopy.
- Assess femoral pulses and Doppler for distal flow.
- Safe Removal Steps:
- Avoid forceful pulling, as this can rupture the iliac or femoral artery.
- Transfer to the operating room for open femoral artery exploration.
- Obtain proximal & distal arterial control, then directly extract the balloon.
- Post-Removal Management:
- Assess for arterial injury; repair if needed.
- Monitor for reperfusion injury and rhabdomyolysis.
Outcome:
- Early OR intervention results in successful removal with minimal vascular damage.
- Delayed intervention may lead to limb loss or life-threatening vascular rupture.
Scenario 3: IABP Malposition (Placed in Femoral Vein Instead of Artery)
Problem:
A 60-year-old in cardiogenic shock after valve surgery has no augmentation on arterial waveform post-IABP insertion. TEE confirms the balloon in the right atrium.
Rectification:
- Immediate Actions:
- Deflate and remove the misplaced IABP immediately.
- Confirm proper arterial cannulation using ultrasound.
- Correct Placement:
- Insert a new IABP in the common femoral artery under fluoroscopy or TEE guidance.
- Ensure positioning in the descending aorta (tip just distal to the left subclavian artery).
- Assess for Complications:
- Venous thromboembolism or iatrogenic right atrial trauma.
Outcome:
- Early recognition leads to successful reimplantation with stable hemodynamics.
- Delayed diagnosis may cause venous thrombosis, atrial injury, or pulmonary embolism.
Scenario 4: Gas Leak or Console Failure
Problem:
A 75-year-old post-CABG patient on IABP develops sudden failure of balloon inflation. The console alarms indicate helium leakage.
Rectification:
- Troubleshooting Steps:
- Check for loose connections in the helium tubing.
- If tubing is intact, replace the IABP console.
- If gas leak persists, consider balloon rupture and remove the device.
- Alternative Hemodynamic Support:
- If weaning is not possible, switch to Impella or VA-ECMO.
Outcome:
- Timely troubleshooting allows continued IABP function.
- If not corrected, the patient may experience hemodynamic instability requiring escalation to advanced mechanical support.
Scenario 5: Limb Ischemia Without IABP Malfunction
Problem:
A 65-year-old with severe cardiogenic shock has an IABP in the left femoral artery. Within 6 hours, the left foot becomes cold, pale, and pulseless.
Rectification:
- Assess Limb Perfusion:
- Doppler ultrasound to check distal pulses.
- CT angiography (if necessary) to assess vascular compromise.
- Management Options:
- If severe ischemia: Remove the IABP and relocate it to the contralateral femoral artery or axillary approach.
- If mild ischemia: Distal perfusion catheter placement (e.g., 7F sidearm sheath for antegrade flow).
- Start heparin infusion to prevent thrombus formation.
- Monitor for Reperfusion Injury:
- Watch for rhabdomyolysis and hyperkalemia after restoring blood flow.
Outcome:
- Early intervention prevents limb loss.
- Delayed recognition may lead to fasciotomy, amputation, or multi-organ failure due to metabolic derangements.
Conclusion
IABP is a life-saving device but comes with risks. Quick recognition of rupture, entrapment, misplacement, console failure, and limb ischemia is crucial for successful outcomes. Using fluoroscopy, ultrasound guidance, and meticulous vascular assessment reduces complications, ensuring better patient safety in critical care and cardiac surgery settings. 🚑💙
Frequently Asked Questions about IABP
Pre-Insertion
1. What are the indications for IABP insertion?
Cardiogenic shock, acute myocardial infarction, post-cardiotomy cardiogenic shock, and bridge to heart transplantation.
2. What are the contraindications for IABP insertion?
Severe aortic regurgitation, aortic aneurysm, severe peripheral vascular disease, and active bleeding.
Insertion and Removal
1. How is an IABP inserted?
Through the femoral artery using a guidewire and fluoroscopic guidance.
1. What are the complications of IABP insertion?
Limb ischemia, bleeding, balloon leak, and vascular complications.
2. How is an IABP removed?
By slowly reducing 1:1 to 1:2 to 1:3 ratio
Understanding how to set up, operate, and adjust the IABP console.
Insertion Techniques: Ensuring safe and efficient catheter insertion.
Monitoring:
Recognizing abnormal pressure waveforms or vital signs.
Troubleshooting:
Knowing how to respond to Technical errors displayed in Console Screen, malfunctioning and their rectification, also severe complications like balloon rupture or limb ischemia.
By understanding the indications, potential complications, and best practices, healthcare professionals can improve the success rate of IABP therapy and ultimately provide better care for patients in need. Proper training, continuous monitoring, and prompt recognition of complications are key to maximizing the benefits of this life-saving intervention.
withdrawing the catheter through the femoral artery sheath and putting pressure about 30 minutes
IABP Therapy
1. How does an IABP work?
By inflating a balloon in the descending aorta during diastole, increasing coronary perfusion and reducing afterload.
2.What are the benefits of IABP therapy?
Improved cardiac output, reduced mortality, and enhanced coronary perfusion.
3.What are the potential complications of IABP therapy?
Limb ischemia, bleeding, balloon leak, and vascular complications.
Monitoring and Troubleshooting
1.How is IABP function monitored?
Through console monitoring, including pressure waveforms, balloon inflation/deflation timing, and alarm systems.
2.What are common issues with IABP therapy?
Balloon leak, catheter kinking, and console malfunction.
3.How are IABP-related complications managed?
Through prompt recognition, catheter adjustment or removal, and supportive care.
Training and Education
1.Who should be trained in IABP use?
Cardiologists,Cardiac Perfusionist ,Cardiothoracic surgeons, critical care physicians,and nursing staff.
2. What topics should IABP training cover?
Device operation, insertion and removal techniques, monitoring, and troubleshooting.
3.How often should IABP training be updated?
Regularly, to reflect advances in technology and changes in clinical practice guidelines.
IABP MCQ Exam
Exam Overview
This exam consists of 150 multiple-choice questions (MCQs) divided into four sections:
- IABP Principles and Mechanics (45 MCQs)
- IABP Operation and Timing (45 MCQs)
- Clinical Applications and Patient Management (30 MCQs)
- Complications and Troubleshooting (30 MCQs)
Each question has a 30-second timer. If you do not answer within 30 seconds, the exam will automatically proceed to the next question, and no marks will be awarded. Click ‘Next’ to proceed or ‘Submit’ on the final question to view results.
Conclusion of Intra-Aortic Balloon Pump (IABP) Therapy
Best Practices for IABP Therapy
Intra-Aortic Balloon Pump therapy remains a cornerstone treatment in critical care, offering temporary circulatory support for patients in cardiogenic shock or heart failure. However, it requires careful consideration of the patient’s condition, meticulous insertion techniques, and constant monitoring to ensure optimal outcomes. visit us for more information at cardiperf.com