Table of Contents:
- Introduction: The Evolving Landscape of Coronary Intervention
- What is Fractional Flow Reserve (FFR)? 2.1 The Physiology Behind FFR 2.2 How FFR Works in Practice
- Fractional Flow Reserve Measurement: A Step-by-Step Guide 3.1 Setting Up for FFR Measurement 3.2 Performing the FFR Assessment 3.3 Interpreting FFR Values: Understanding the Significance
- The Clinical Applications of FFR: Guiding Critical Decisions 4.1 FFR in Stable Coronary Artery Disease 4.2 FFR in Acute Coronary Syndrome (ACS) 4.3 FFR for Evaluating Intermediate Lesions 4.4 Coronary Artery Disease and the Heart Team Approach
- FFR vs. Angiography: Enhancing Diagnostic Accuracy
- FFR vs. iFR: Exploring the Nuances of Physiological Assessment
- The Impact of FFR on Patient Outcomes: Evidence-Based Insights 7.1 Reducing Major Adverse Cardiac Events (MACE) 7.2 Improving Stenting Outcomes 7.3 Long-Term Benefits of FFR-Guided Interventions
- FFR in Specific Clinical Scenarios 8.1 FFR in Multivessel Disease 8.2 FFR in Left Main Disease 8.3 FFR in Bypass Grafts
- Integrating FFR into Clinical Practice: Best Practices and Considerations 9.1 Training and Competency in FFR Measurement 9.2 Cost-Effectiveness of FFR Implementation 9.3 Overcoming Challenges in FFR Adoption
- Advancements and Future Directions in FFR Technology
- Frequently Asked Questions (FAQs)
- Conclusion: FFR – A Cornerstone of Modern Coronary Interventions
1. Introduction: The Evolving Landscape of Coronary Intervention
The management of coronary artery disease (CAD) has undergone a dramatic transformation in recent decades. While angiography has long served as the gold standard for visualizing coronary anatomy, it provides limited information about the functional significance of coronary stenoses. This is where Fractional Flow Reserve (FFR) has emerged as a game-changing tool. FFR empowers clinicians with precise physiological data, enabling more informed decision-making in percutaneous coronary intervention (PCI) and ultimately improving patient outcomes.
2. What is Fractional Flow Reserve (FFR)?
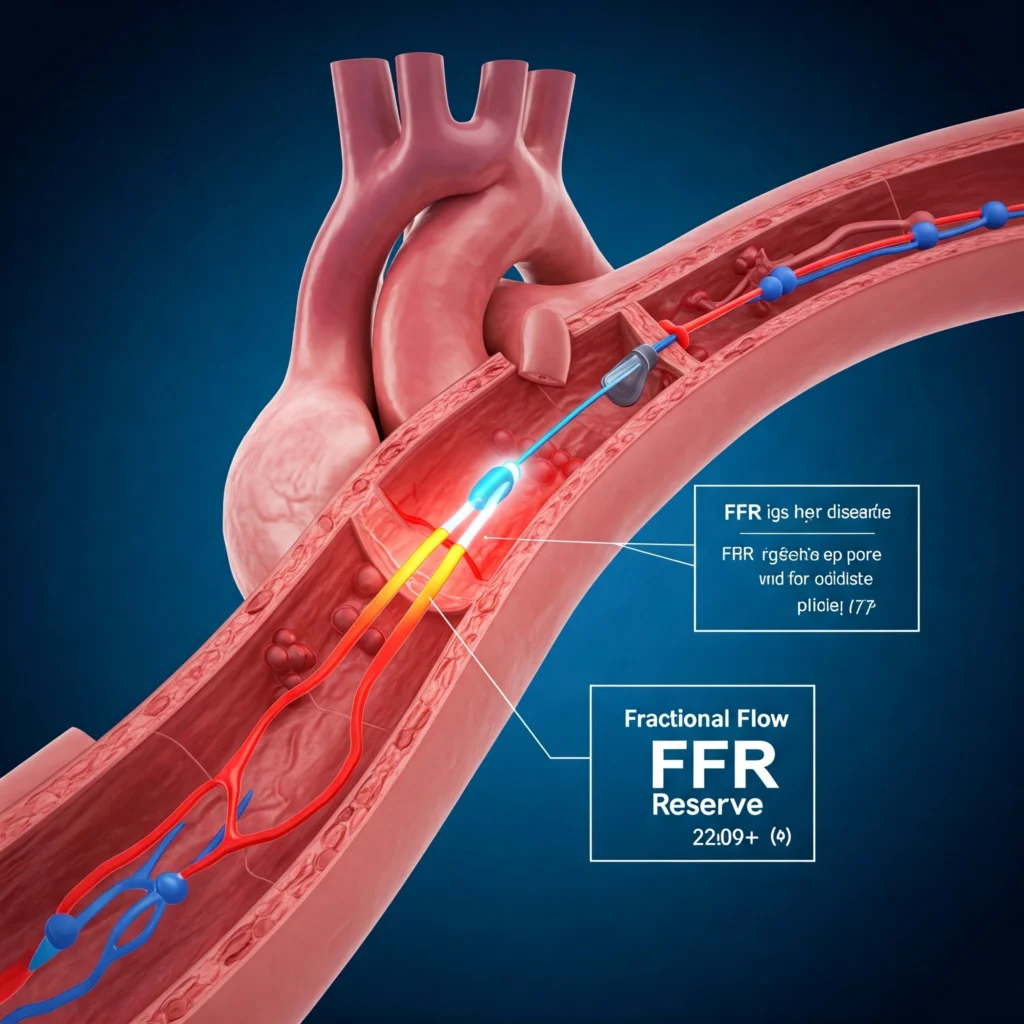
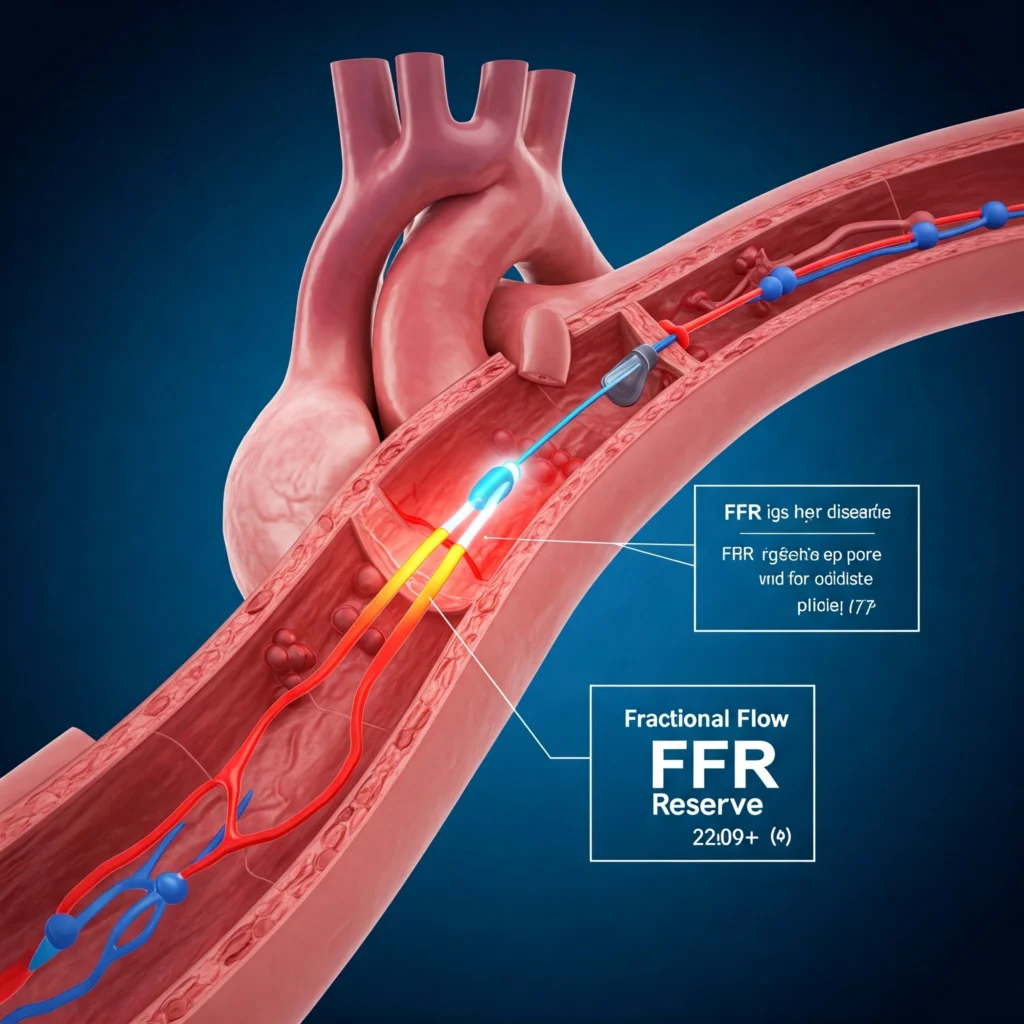
Fractional Flow Reserve (FFR) is a pressure-derived measurement that quantifies the functional significance of a coronary stenosis by assessing the impact of the narrowing on downstream blood flow. It essentially tells us how much the blockage is impeding blood flow to the heart muscle.
2.1 The Physiology Behind FFR
FFR is based on the principle that blood flow to the myocardium is directly proportional to the pressure gradient across a coronary stenosis. A significant stenosis will create a pressure drop, reducing blood flow to the downstream myocardium. FFR measures this pressure drop, providing a quantitative assessment of the functional severity of the lesion.
2.2 How FFR Works in Practice
During a coronary angiogram, a specialized pressure wire is advanced across the coronary stenosis. The pressure is measured both proximal and distal to the blockage. The FFR is calculated as the ratio of the mean distal coronary pressure (Pd) to the mean proximal coronary pressure (Pa) during maximal hyperemia.
3. Fractional Flow Reserve Measurement: A Step-by-Step Guide
3.1 Setting Up for FFR Measurement
The FFR procedure is typically performed during a diagnostic coronary angiogram. After the guide catheter is engaged, the pressure wire is advanced… (Detailed explanation of the procedure, including equipment, calibration, and wire placement.)
3.2 Performing the FFR Assessment
Once the wire is positioned, hyperemia is induced… (Detailed explanation of inducing hyperemia, including pharmacological agents and their effects.)
3.3 Interpreting FFR Values: Understanding the Significance
FFR values range from 0 to 1. An FFR value of ≤0.80 is generally considered functionally significant, indicating that the stenosis is causing myocardial ischemia. (Explanation of FFR thresholds and their clinical implications.)
4. The Clinical Applications of FFR: Guiding Critical Decisions
4.1 FFR in Stable Coronary Artery Disease
FFR plays a crucial role in determining which lesions in stable CAD warrant intervention. (Discussion of FFR’s role in guiding PCI decisions in stable angina.)
4.2 FFR in Acute Coronary Syndrome (ACS)
The use of FFR in ACS can be more complex… (Discussion of the challenges and benefits of FFR in the setting of unstable angina and myocardial infarction.)
4.3 FFR for Evaluating Intermediate Lesions
FFR is particularly valuable in assessing intermediate lesions (those with 40-70% stenosis) where the functional significance is uncertain.
4.4 Coronary Artery Disease and the Heart Team Approach
FFR data provides objective physiological information that helps the Heart Team… (Discussion of how FFR contributes to collaborative decision-making.)
5. FFR vs. Angiography: Enhancing Diagnostic Accuracy
Angiography provides a detailed anatomical view of the coronary arteries, but it does not directly assess the functional impact of stenoses. FFR complements angiography by providing crucial physiological information… (Detailed comparison of FFR and angiography, highlighting the strengths and limitations of each.)
6. FFR vs. iFR: Exploring the Nuances of Physiological Assessment
Instantaneous Wave-Free Ratio (iFR) is another physiological assessment tool… (Detailed comparison of FFR and iFR, including the advantages and disadvantages of each.)
7. The Impact of FFR on Patient Outcomes: Evidence-Based Insights
7.1 Reducing Major Adverse Cardiac Events (MACE)
Numerous studies have demonstrated that FFR-guided PCI… (Presentation of clinical trial data showing the benefits of FFR in reducing MACE.)
7.2 Improving Stenting Outcomes
FFR helps ensure that stents are placed in functionally significant lesions… (Discussion of how FFR improves stent placement and reduces the risk of restenosis.)
7.3 Long-Term Benefits of FFR-Guided Interventions
The long-term benefits of FFR-guided PCI include… (Discussion of the long-term impact of FFR on patient survival and quality of life.)
8. FFR in Specific Clinical Scenarios
8.1 FFR in Multivessel Disease
FFR can be particularly useful in multivessel disease… (Discussion of the role of FFR in guiding revascularization strategies in patients with multiple coronary lesions.)
8.2 Coronary Artery Disease in Left Main Disease
The assessment of left main coronary artery stenosis requires careful consideration… (Discussion of the use of FFR in evaluating left main disease.)
8.3 FFR in Bypass Grafts
FFR can be used to assess the functional significance of stenoses in bypass grafts… (Discussion of the application of FFR in patients with prior coronary artery bypass grafting.)
9. Integrating FFR into Clinical Practice: Best Practices and Considerations
9.1 Training and Competency in FFR Measurement
Proper training and competency are essential for accurate FFR measurement and interpretation… (Discussion of training requirements and best practices for FFR procedures.)
9.2 Cost-Effectiveness of FFR Implementation
While the FFR procedure adds some cost… (Analysis of the cost-effectiveness of FFR-guided PCI, considering the long-term benefits.)
9.3 Overcoming Challenges in FFR Adoption
Despite the strong evidence supporting its use… (Discussion of the barriers to wider adoption of FFR and strategies for overcoming them.)
10. Advancements and Future Directions in FFR Technology
Ongoing research is focused on… (Discussion of advancements in FFR technology, such as wireless FFR and new physiological indices.)
11. Frequently Asked Questions (FAQs)
Here are 10 frequently asked questions about Fractional Flow Reserve (FFR), complete with answers:
- What is fractional flow reserve (FFR) and how does it work? Fractional Flow Reserve (FFR) is a physiological measurement used during coronary angiography to determine the functional significance of a coronary artery stenosis (narrowing). It measures the pressure difference across the blockage to assess how much it’s limiting blood flow to the heart muscle. A specialized pressure wire is placed across the narrowing, and the ratio of pressure distal to the stenosis (Pd) to the pressure proximal to the stenosis (Pa) is calculated during maximal hyperemia (increased blood flow). This ratio is the FFR value.
- How is fractional flow reserve (FFR) measured during angiography? During a coronary angiogram, after the guide catheter is positioned, a pressure-sensitive guidewire is advanced across the coronary stenosis. Pressure is measured both before and after the blockage. Hyperemia is then induced, either through exercise or with medication (like adenosine), to maximize blood flow. The FFR is calculated as the ratio of distal to proximal pressure during hyperemia.
- What are the benefits of using FFR in coronary artery disease? FFR helps cardiologists determine which coronary narrowings are actually causing ischemia (reduced blood flow) and thus warrant intervention (like stenting or bypass surgery). This leads to more appropriate treatment decisions, reduces unnecessary procedures, and improves patient outcomes. It also helps in assessing the functional significance of intermediate lesions (40-70% stenosis) where angiography alone can be inconclusive.
- Is fractional flow reserve (FFR) more accurate than angiography alone? Yes, FFR provides functional information that angiography alone cannot. Angiography shows the anatomy of the coronary arteries (the degree of narrowing), but FFR shows the functional impact of the narrowing on blood flow. FFR helps determine if a narrowing is actually causing a reduction in blood flow to the heart muscle, even if it appears significant on angiography.
- What is a normal FFR value and what does it mean? An FFR value of 1.0 represents normal blood flow. An FFR value ≤0.80 is generally considered functionally significant, meaning the narrowing is causing ischemia. Values between 0.80 and 1.0 are in a gray zone, and clinical judgment is required.
- What are the risks associated with fractional flow reserve (FFR)? FFR is generally a safe procedure. The risks are similar to those of a standard coronary angiogram, including the possibility of bleeding, hematoma, or allergic reaction to the contrast dye. There is a small risk of coronary artery dissection or spasm, but these complications are rare.
- How long does a fractional flow reserve (FFR) procedure take? The FFR measurement itself adds only a few minutes to the overall angiogram procedure. The total procedure time depends on the complexity of the case, but it’s typically similar to a standard diagnostic angiogram.
- Does insurance cover fractional flow reserve (FFR) testing? Most insurance companies cover FFR testing when it is medically necessary. However, it’s always best to check with your insurance provider to confirm coverage and any specific requirements.
- What happens if my FFR value is low (≤0.80)? A low FFR value indicates that the coronary narrowing is functionally significant and is likely causing ischemia. Your cardiologist will use this information, along with other clinical factors, to recommend the most appropriate treatment, which may include medical therapy, stenting (PCI), or coronary artery bypass grafting (CABG).
- How does FFR improve outcomes after coronary intervention?
FFR-guided PCI helps ensure that stents are placed in lesions that are truly causing ischemia. This leads to better symptom relief, improved blood flow to the heart muscle, and a reduced risk of future cardiac events. Studies have shown that FFR-guided PCI is associated with lower rates of MACE (major adverse cardiac events) compared to angiography-guided PCI alone.
12. Conclusion: FFR – A Cornerstone of Modern Coronary Interventions
Fractional Flow Reserve (FFR) has become an indispensable tool in the modern management of coronary artery disease. By providing objective physiological data, FFR empowers cardiologists to make informed decisions about which lesions warrant intervention, leading to more appropriate treatment strategies, improved patient outcomes, and a reduction in unnecessary procedures. As technology continues to advance, FFR is likely to play an even greater role in the future of coronary interventions. for latest update regarding cardiac perfusion sciences visit us at cardiperf.com