Beating heart surgery, also known as Off-Pump Coronary Artery Bypass Grafting (OPCAB), is a revolutionary technique in cardiac surgery. Unlike traditional coronary artery bypass surgery, which involves stopping the heart, OPCAB allows surgeons to operate on a beating heart, reducing potential complications and promoting faster recovery.
What is Beating-Heart Coronary Artery Bypass Surgery?
Beating-heart coronary artery bypass surgery is a procedure designed to treat coronary artery disease (CAD) by bypassing blocked arteries without stopping the heart. CAD occurs when plaque buildup in the coronary arteries restricts blood flow, leading to chest pain (angina) or heart attacks.
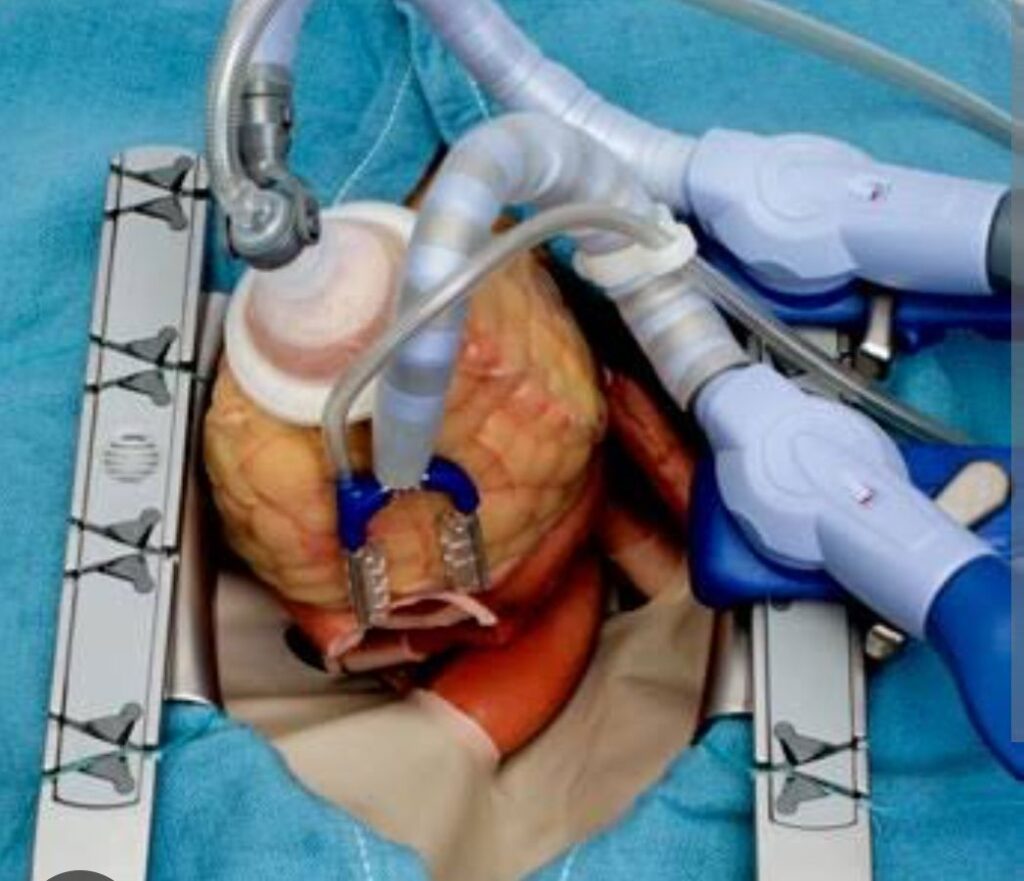
In this approach, specialized stabilizing devices are used to hold specific areas of the beating heart steady, enabling precise grafting. The rest of the heart continues to beat normally, eliminating the need for a heart-lung machine.
How is Beating-Heart Bypass Surgery Performed?
- Preparation: The patient is placed under general anesthesia, and the chest is opened to expose the heart.
- Stabilization: Mechanical devices like the Octopus stabilizer and Archen stabilizer are used to hold the heart steady. A starfish blower-mister may also be employed to clear the surgical field of blood and improve visibility.
- Grafting: Surgeons use veins or arteries, often from the leg or chest, to create bypasses around the blocked arteries. Intra-coronary shunts are sometimes used to maintain blood flow to the heart muscle during the grafting process.
- Closure: After the grafts are secured, the chest is closed, and the patient is moved to recovery.
This procedure typically takes 3 to 5 hours, depending on the complexity and number of bypasses required.
Benefits of Beating-Heart Bypass Surgery
Beating-heart surgery offers several advantages over traditional on-pump coronary artery bypass surgery:
- Reduced complications: Avoiding the heart-lung machine decreases risks like stroke, blood clots, and organ dysfunction.
- Shorter recovery time: Patients often recover more quickly due to less trauma to the heart and body.
- Lower need for blood transfusions: Natural blood circulation is maintained during surgery.
- Less stress on the body: Particularly beneficial for elderly patients or those with multiple health issues.
Candidates for Beating-Heart Bypass Surgery
This approach is suitable for:
- Patients at higher risk of complications from the heart-lung machine.
- Those with stable coronary artery disease and fewer blockages.
- Patients with coexisting conditions such as kidney disease or a history of stroke.
Preparing for Off-Pump Bypass Surgery
Before the procedure, patients undergo thorough evaluations, including:
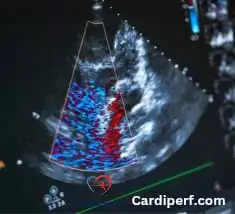
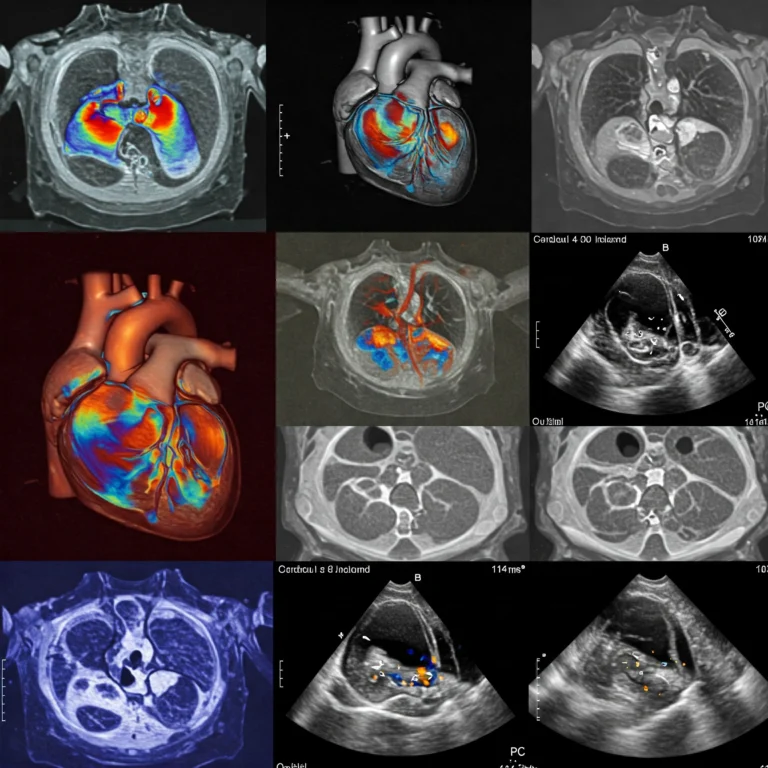
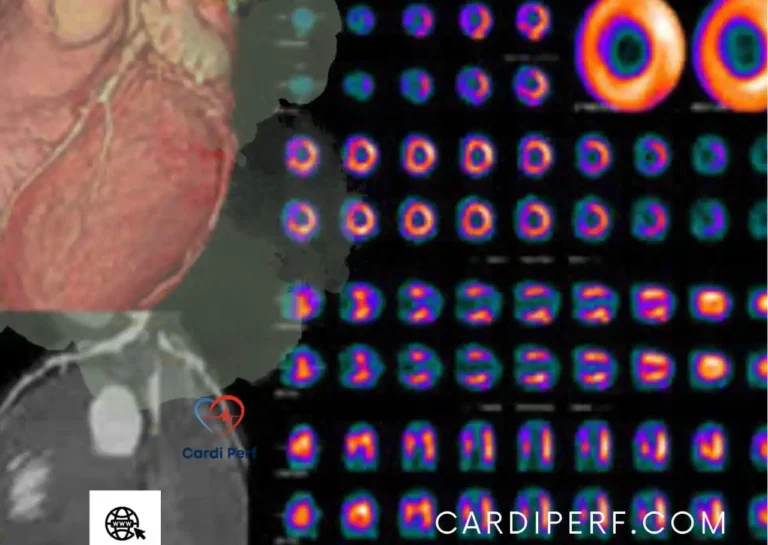
- Blood tests, ECG, and imaging: To assess heart health and identify blockages.
- Medication adjustments: Patients may need to stop taking blood thinners or other medications before surgery.
- Lifestyle preparation: Smoking cessation and healthy eating can improve surgical outcomes.
What Happens During Off-Pump Bypass Surgery?
During the procedure:
- The heart continues to beat while the surgeon works on individual arteries.
- Stabilizing devices minimize movement in the operating area.
- Grafts are placed to bypass blockages and restore blood flow.

Post-Surgery Recovery
After the surgery, patients typically:
- Spend time in the intensive care unit (ICU) for monitoring.
- Begin walking and light activities within days.
- Fully recover within 6 to 12 weeks, depending on their overall health.
Risks and Complications
While off-pump bypass surgery is generally safe, potential risks include:
- Bleeding or infection.
- Stroke or heart attack.
- Arrhythmias (irregular heartbeats).
On-Pump vs. Off-Pump Bypass Surgery
The choice between on-pump and off-pump surgery depends on the patient’s condition:
- On-pump surgery: Provides a still heart, which may be advantageous in complex cases.
- Off-pump surgery: Reduces complications and recovery time, particularly for high-risk patients.
When to Seek Medical Attention After Surgery
Contact your doctor if you experience:
- Severe chest pain or shortness of breath.
- Signs of infection, such as fever or redness around the surgical site.
- Irregular heartbeats or fainting.
Coronary Artery Disease and Chest Pain
CAD is a leading cause of chest pain and heart attacks. Lifestyle changes, medications, and surgical interventions like beating-heart bypass surgery can significantly improve quality of life and longevity.
The Future of Beating-Heart Surgery
Beating-heart bypass surgery is increasingly recognized as a safer, more patient-friendly alternative to traditional methods. By reducing the risks associated with the heart-lung machine, it has become an essential tool in modern cardiac surgery.
FAQs About Beating-Heart Bypass Surgery
1. What is the main difference between on-pump and off-pump bypass surgery?
On-pump surgery uses a heart-lung machine to take over the function of the heart and lungs during surgery, while off-pump surgery allows the heart to continue beating, avoiding the machine.
2. How long does it take to recover from beating-heart bypass surgery?
Recovery typically takes 6 to 12 weeks, but it can vary depending on individual health and the complexity of the surgery.
3. What devices are used in beating-heart surgery?
Devices like the Octopus stabilizer, Archen stabilizer, starfish blower-mister, and intra-coronary shunts are employed to stabilize the heart and maintain blood flow during surgery.
4. Who is a good candidate for beating-heart surgery?
Patients with stable coronary artery disease, those at high risk of complications from the heart-lung machine, or individuals with coexisting conditions like kidney disease are ideal candidates.
5. Are there risks associated with off-pump surgery?
While generally safe, risks include bleeding, infection, arrhythmias, or, in rare cases, stroke or heart attack.
6. Is beating-heart bypass surgery widely available?
Yes, it is increasingly available at major cardiac centers due to its proven benefits and advancements in surgical techniques.
Additional Questions a Patient or Relative May Have About Triple Vessel Artery Disease
1. What is triple vessel artery disease?
It refers to significant blockages in all three major coronary arteries, requiring comprehensive treatment like bypass surgery.
2. Can triple vessel disease be treated without surgery?
In some cases, medications or stent placements may be considered, but bypass surgery is often the most effective treatment for severe blockages.
3. How does bypass surgery help with triple vessel disease?
By redirecting blood flow around the blocked arteries using grafts, bypass surgery restores proper blood circulation to the heart muscle.
4. What lifestyle changes are recommended after surgery?
Patients should adopt a heart-healthy diet, exercise regularly, avoid smoking, and manage stress to prevent future complications.
5. Are there alternatives to beating-heart surgery for triple vessel disease?
Traditional on-pump bypass surgery or advanced stenting techniques may be considered based on the patient’s specific condition.
6. How can family members support a patient undergoing bypass surgery?
Providing emotional support, helping with lifestyle changes, and attending follow-up appointments are vital for a successful recovery.
Conclusion
For patients with coronary artery disease, beating-heart coronary artery bypass surgery offers a safer, less invasive option with quicker recovery times. If you or a loved one is considering bypass surgery, consult your cardiac surgeon about whether the off-pump approach is right for you.
Stay informed and heart-healthy with the latest insights on cardiac care at CardiPerf.com.