Aortic Dissection During Cardiac Surgery: A Collaborative Approach to Management Among Anesthesiologists, Cardiac Surgeons, Perfusionists, and Nursing Team
In the high-stakes world of cardiac surgery, effective teamwork among anesthesiologists, cardiac surgeons, perfusionists, and nursing staff is critical to ensure patient safety and optimize outcomes. One of the most challenging and potentially life-threatening complications that can occur during cardiac surgery is intraoperative aortic dissection. This rare yet catastrophic event requires the rapid, coordinated efforts of the entire surgical team, from diagnosis to intervention.
This blog post delves into the roles and responsibilities of each team member—anesthesiologists, cardiac surgeons, perfusionists, and nurses—and explores how their combined expertise can avert disaster when aortic dissection occurs in the operating room. By fostering collaboration and communication, the team can significantly improve patient survival rates during this critical emergency.

Aortic Dissection in Cardiac Surgery: A High-Risk Event
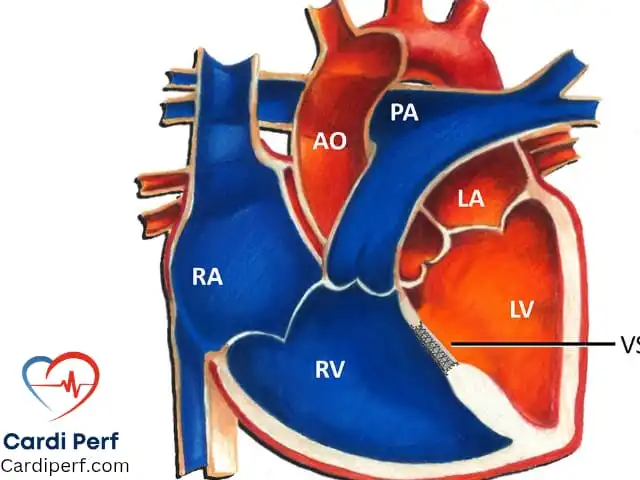
Aortic dissection is a tear in the inner layer (intima) of the aortic wall that allows blood to flow between the layers of the artery. This leads to the formation of a false lumen, which can obstruct blood flow to vital organs, causing severe complications such as stroke, myocardial infarction, or even death. During cardiac surgery, aortic dissection can occur due to various factors, including trauma from aortic cannulation, pre-existing aortic disease, or pressure fluctuations during cardiopulmonary bypass (CPB).
Intraoperative aortic dissection has an incidence rate of about 0.06-0.16%, but it carries a high mortality rate of up to 48% if not managed promptly. The key to saving the patient lies in the swift and effective response from the entire multidisciplinary team.
The Crucial Roles of the Surgical Team
The team working in the operating room during cardiac surgery needs to work seamlessly to manage complications like aortic dissection. Let’s break down the unique and equally important contributions of each team member.
1. Cardiac Surgeons: First Responders to the Crisis
Cardiac surgeons are often the first to recognize potential complications during surgery, including aortic dissection. The surgeon’s ability to remain calm, quickly assess the situation, and take immediate corrective action is critical. Here’s how the surgeon contributes:
- Initial Assessment and Diagnosis: Surgeons must carefully monitor for signs of dissection, such as difficulty achieving adequate flow, abnormal back bleeding from the cannula, or discrepancies in blood pressure measurements. When a dissection is suspected, the surgeon will call for imaging (e.g., transesophageal echocardiography) to confirm the diagnosis.
- Cannulation and Arterial Access: If aortic dissection is diagnosed, the surgeon’s first task is to establish alternative arterial cannulation, often through the femoral artery. This requires quick thinking and dexterity to switch perfusion from the aorta to a safer cannulation site while maintaining hemodynamic stability.
- Aortic Repair: The surgeon must then repair the aorta, typically through circulatory arrest, which involves cooling the patient to a hypothermic state to protect vital organs during the repair. The surgeon will perform a detailed inspection of the aortic root, excise any intimal tears, and perform graft replacement or a hemiarch anastomosis depending on the extent of the dissection.
2. Anesthesiologists: The Guardians of Hemodynamics
Anesthesiologists play a pivotal role in managing the patient’s overall stability, especially during high-risk events like aortic dissection. Their primary responsibilities in this scenario include:
- Hemodynamic Monitoring: The anesthesiologist is responsible for continuously monitoring the patient’s blood pressure, heart rate, and oxygenation levels. Changes in arterial pressure, particularly discrepancies between radial and central aortic pressures, could signal aortic dissection. The anesthesiologist must ensure that these changes are promptly communicated to the surgeon and perfusionist.
- Sedation and Ventilation: In cases of aortic dissection, general anesthesia is critical. The anesthesiologist must adjust sedation levels to ensure the patient is stable and relaxed during potentially stressful procedures like femoral artery cannulation and aortic repair. Additionally, they are responsible for managing ventilation, ensuring that oxygenation and carbon dioxide levels are controlled, especially when circulatory arrest is necessary.
- Managing Circulatory Arrest: If circulatory arrest is needed, anesthesiologists are responsible for carefully regulating the temperature and ensuring the patient is adequately cooled. They work in tandem with the surgeon to manage rewarming, as well as monitor for signs of ischemia or neurological deficits.
3. Perfusionists: The Heart-Lung Machine Experts
Perfusionists are at the center of managing cardiopulmonary bypass during aortic dissection. Their ability to troubleshoot and adjust the heart-lung machine is essential for stabilizing the patient during an emergency. Here’s how they contribute:
- Monitoring and Adjusting Flow Rates: Perfusionists must closely monitor the flow rates and pressures of the CPB machine. If the dissection causes issues like high arterial inflow pressure, perfusionists will be the first to notice and communicate this to the surgeon and anesthesiologist. Rapid adjustment of the pump to ensure adequate perfusion is vital.
- Switching Arterial Cannulation: If an alternative arterial access, such as femoral cannulation, is needed, perfusionists will quickly change over the flow and ensure that the patient remains well-perfused. They must also monitor for air embolism and maintain appropriate de-airing during this transition.
- Temperature Management: Perfusionists play a crucial role in cooling the patient during circulatory arrest. They adjust the temperature of the CPB machine to achieve the desired hypothermic state, ensuring that the brain and other organs are protected from ischemic damage during the surgical repair of the aorta.
4. Nurses: The Unsung Heroes of Support and Coordination
Nurses, both scrub and circulating, form the backbone of the operating room team. Their roles are multifaceted and essential to the smooth running of the surgical procedure, especially during an emergency like aortic dissection.
- Surgical Assistance: Scrub nurses assist the surgeon by providing the necessary instruments, ensuring sterility, and preparing the surgical site for any additional incisions (e.g., for femoral cannulation). They are also responsible for anticipating the surgeon’s needs, such as having extra sutures ready or assisting in the placement of cardioplegia catheters.
- Patient Monitoring and Communication: Circulating nurses are responsible for managing the overall environment, including the patient’s position, maintaining sterile fields, and communicating with other hospital teams, such as the blood bank for any necessary transfusions. They ensure that all protocols are followed and that the team is ready for any sudden changes in the surgical flow.
- Inventory and Equipment Management: Nurses ensure that all necessary equipment is available, such as additional cannulas, grafts, and specialized instruments needed for the repair of the aorta. They also help manage emergency supplies in cases where blood loss is substantial.
The Importance of Teamwork: How Collaboration Saves Lives
The successful management of aortic dissection during cardiac surgery is a direct result of effective communication and collaboration between anesthesiologists, cardiac surgeons, perfusionists, and nursing staff. Each team member must be proactive, alert, and willing to assist their colleagues in a crisis.
In the case of aortic dissection, it is not only the surgeon’s skill that saves the patient, but also the quick, precise interventions by the anesthesiologist, perfusionist, and nursing team. The importance of clear communication cannot be overstated. From the first signs of trouble to the final repair of the aorta, each team member’s contribution is essential.
Conclusion
Aortic dissection during cardiac surgery, though rare, is a high-risk complication that demands a quick and coordinated response from the entire operating room team. Anesthesiologists, cardiac surgeons, perfusionists, and nurses must all work together seamlessly to stabilize the patient, manage circulatory arrest, and perform the necessary repairs to the aorta. In these high-pressure situations, effective teamwork is not just a luxury—it is the key to saving lives.
By fostering a culture of collaboration and mutual respect, the surgical team can navigate even the most challenging situations and deliver optimal patient outcomes. Whether you are a cardiac surgeon, anesthesiologist, perfusionist, or nurse, your role in managing aortic dissection is vital to the success of the procedure and the survival of the patient. For update information visit us at cardiperf.com.