Air embolism during cardiopulmonary bypass (CPB) is a potentially catastrophic event that can lead to severe neurological and cardiovascular complications. Despite advanced safety features in modern CPB machines, accidental air entry into the circuit can still occur, primarily due to human error or system malfunctions. This article explores a real-world case of air embolism, its causes, management strategies, and preventative measures, serving as a crucial guide for cardiac surgeons, perfusionists, and anesthesiologists.
A Real-Life Nightmare in the OR
“One small mistake in the OR—cutting off a simple air filter—almost cost a patient her life. This is how we stopped disaster in its tracks.”
Case Presentation
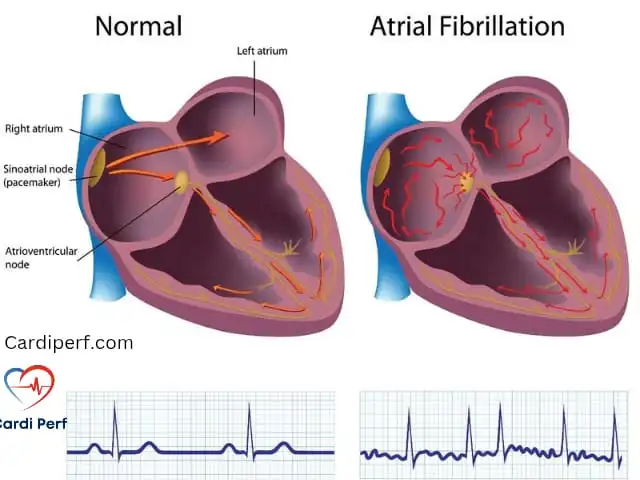
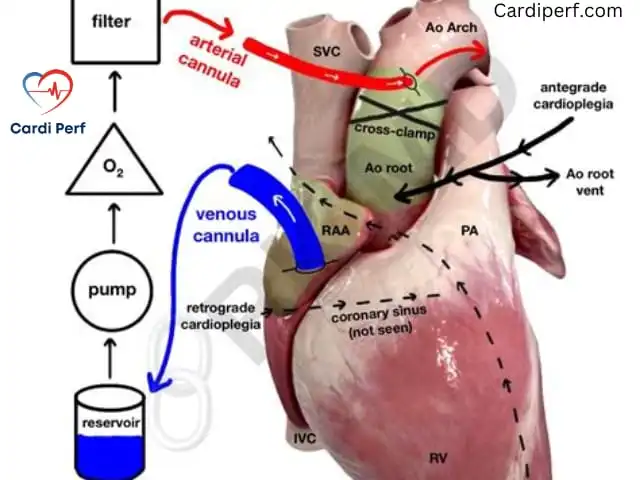
A 75-year-old female with severe mitral regurgitation due to A2/A3 segment prolapse was scheduled for mitral valve repair, left atrial appendage amputation, and a Maze procedure. The patient was placed on CPB with central aortic cannulation and bicaval venous cannulation. Standard antegrade cold blood cardioplegia was used to arrest the heart.
To maintain a bloodless surgical field, a floppy sucker was placed in the left superior pulmonary vein to manage pulmonary venous return. However, it was ineffective, leading the team to remove the protective air filter to increase suction. This ultimately resulted in inadvertent air entry into the left side of the heart, leading to cerebral air embolism.
Understanding the Problem: Causes of Air Embolism
Air embolism in cardiac surgery can occur due to several factors:
- Reversal of Flow in Suction Lines: Removing protective air filters from vent lines can allow air entry if flow is accidentally reversed.
- Low Venous Reservoir Volume: If the venous reservoir drops too low, air can be aspirated into the arterial circuit.
- Malfunctioning Alarms: If air detection alarms fail, unnoticed air bubbles can be pumped into the patient.
- Accidental Shunt Openings: Improperly managed shunts can allow unintended air flow into the left heart.
- Improper De-Airing Procedures: If air is not meticulously evacuated from the heart before removing the cross-clamp, embolism risk increases.
Immediate Management of Air Embolism
When air embolism occurs, rapid intervention is critical to mitigate neurological damage. The following steps should be taken immediately:
1. Halt CPB and Stop Air Entry
- Immediately stop perfusion and clamp arterial and venous lines.
- Identify and eliminate the source of air entry (e.g., suction line errors, shunt mismanagement).
2. Positioning for Air Clearance
- Place the patient in a steep Trendelenburg position (head down) to prevent air migration to cerebral circulation.
- Ensure 100% oxygen administration via the ventilator to accelerate nitrogen washout.
3. De-Air the Circuit and Patient
- Apply suction to the aortic root vent to extract air from the left heart and ascending aorta.
- Loosen the aortic cannulation purse strings and allow air to escape.
- If air is in the arterial circuit, remove the aortic cannula, de-air it, and reconnect it after ensuring complete air evacuation.
4. Retrograde Cerebral Perfusion
- Establish retrograde brain perfusion by diverting arterial flow through the superior vena cava (SVC) cannula at 300 mL/min.
- Monitor for air bubbles exiting through the aortic root vent or aortic cannulation site.
5. Cooling and Neuroprotection
- Lower body temperature to 28°C to reduce cerebral metabolic demand.
- Administer steroids, barbiturates, and/or mannitol for neuroprotection.
- Maintain deep anesthesia for 24-48 hours postoperatively.
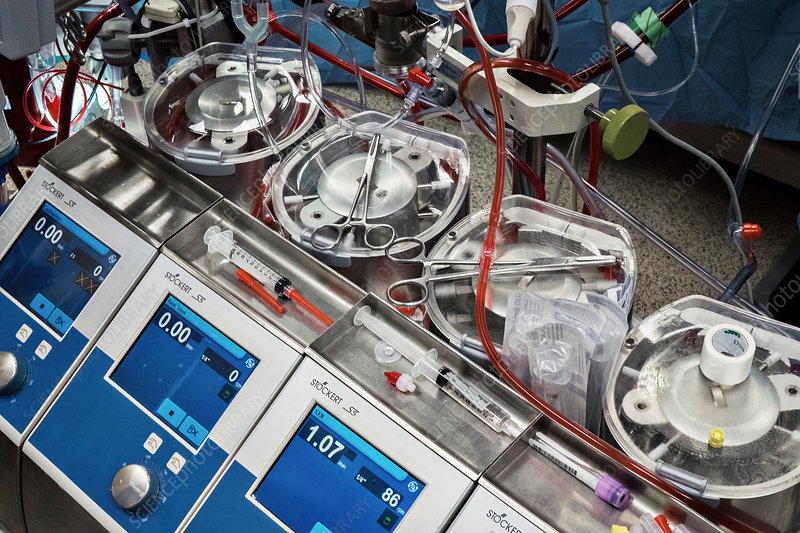
The Crucial Role of the Perfusionist in Air Embolism Prevention
Perfusionists play a central role in preventing air embolism and ensuring patient safety during CPB. Key responsibilities include:
1. Continuous Monitoring and Alarm System Management
- Regularly check venous reservoir levels to avoid air entrainment.
- Ensure air bubble detection alarms are active and functioning.
2. Maintaining Circuit Integrity
- Inspect all connections, cannulas, and shunts before and during bypass.
- Confirm that air filters on vent and suction lines remain intact.
3. Safe De-Airing Techniques
- Use CO2 flushing techniques to reduce intracardiac air retention.
- Keep root suction active during de-airing and ensure the patient is in Trendelenburg position.
4. Communication and Team Coordination
- Maintain clear, real-time communication with the surgical and anesthesia teams.
- Be prepared to initiate emergency protocols immediately if air is detected.
Preventative Strategies: Avoiding Air Embolism
Prevention is always superior to treatment. Here are essential strategies to minimize the risk of air embolism:
- Strict Adherence to Vent Line Safety Protocols
- Never remove protective air filters from vent lines.
- Ensure vent suction lines are properly oriented to prevent reversal of flow.
- Maintain Adequate Venous Reservoir Volume
- Monitor reservoir levels continuously to prevent air aspiration.
- Utilize CPB alarms and sensors to detect low reservoir conditions early.
- Meticulous De-Airing Before Cross-Clamp Removal
- Use Trendelenburg positioning and controlled ventilation with Valsalva maneuvers to expel air.
- Maintain root suction during de-airing to capture any residual air.
- Advanced CPB Safety Features
- Utilize air detection and automatic circuit shutoff mechanisms.
- Consider incorporating CO2 flushing to minimize intracardiac air persistence.
Frequently Asked Questions (FAQs)
- What is an air embolism?
- An air embolism occurs when air enters the bloodstream, potentially blocking blood flow and causing severe complications.
- How does air enter the CPB circuit?
- Common causes include low venous reservoir levels, reversed suction line flow, and improperly de-aired cannulas.
- What are the symptoms of air embolism?
- Neurological deficits, hypotension, ST changes, and loss of consciousness.
- How is air embolism diagnosed intraoperatively?
- Detection via transesophageal echocardiography (TEE) and observation of air bubbles in arterial lines.
- How can perfusionists prevent air embolism?
- By maintaining reservoir volume, using air detection sensors, and following strict de-airing protocols.
- What is the role of the Trendelenburg position?
- It helps prevent air migration to cerebral circulation and facilitates air removal.
- Why is retrograde cerebral perfusion important?
- It helps flush air out of cerebral circulation, reducing the risk of neurological injury.
- Can hyperbaric oxygen therapy be used postoperatively?
- Yes, it may be considered to enhance nitrogen washout and minimize neurological damage.
- What medications help in air embolism management?
- Steroids, barbiturates, and mannitol can aid in neuroprotection and cerebral edema reduction.
- How can I learn more about CPB safety?
- Visit CardiPerf.com for in-depth resources on perfusion science and patient safety.
Disclaimer
This article is for educational purposes only and should not replace professional medical advice. Always consult experienced clinicians when managing air embolism cases.
About Cardiperf.com
Cardiperf.com is a leading resource for cardiac perfusionists, surgeons, and healthcare providers, offering cutting-edge insights into perfusion science, cardiac surgery techniques, and patient care strategies. Stay updated with the latest advancements in the field by visiting our website cardiperf.com