Table of Contents:
- Introduction: Recognizing the Urgency of Acute Coronary Syndrome
- Understanding Acute Coronary Syndrome: A Spectrum of Conditions 2.1. Unstable Angina 2.2. Myocardial Infarction (Heart Attack) 2.2.1 STEMI (ST-Elevation Myocardial Infarction) 2.2.2 NSTEMI (Non-ST-Elevation Myocardial Infarction)
- Deciphering the Symptoms of Acute Coronary Syndrome: Time is Muscle
- The Crucial Role of Rapid Diagnosis in Acute Coronary Syndrome 4.1. Electrocardiogram (ECG) 4.2. Cardiac Biomarkers 4.3. Other Diagnostic Tests
- Evidence-Based Treatment Strategies for Acute Coronary Syndrome: Restoring Blood Flow 5.1. Immediate Management 5.2. Pharmacological Interventions 5.3. Revascularization Procedures 5.3.1. Percutaneous Coronary Intervention (PCI) 5.3.2. Thrombolytic Therapy 5.3.3. Coronary Artery Bypass Grafting (CABG)
- Risk Factors for Acute Coronary Syndrome: Identifying Vulnerable Individuals
- Empowering Prevention: Reducing the Risk of Acute Coronary Syndrome
- Managing Acute Coronary Syndrome: A Collaborative Approach
- Prognosis and Long-Term Effects of Acute Coronary Syndrome
- Frequently Asked Questions (FAQs)
- Conclusion: Advancing ACS Care Through Knowledge and Action
1. Introduction: Recognizing the Urgency of Acute Coronary Syndrome
Acute Coronary Syndrome (ACS) represents a spectrum of life-threatening conditions that demand immediate medical attention. Characterized by a sudden reduction in blood flow to the heart, ACS encompasses unstable angina, non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI) 1 – all requiring rapid diagnosis and intervention to minimize myocardial damage and improve patient outcomes. This comprehensive guide is designed for healthcare professionals to enhance their understanding of ACS, from recognizing its symptoms to implementing evidence-based treatment strategies.
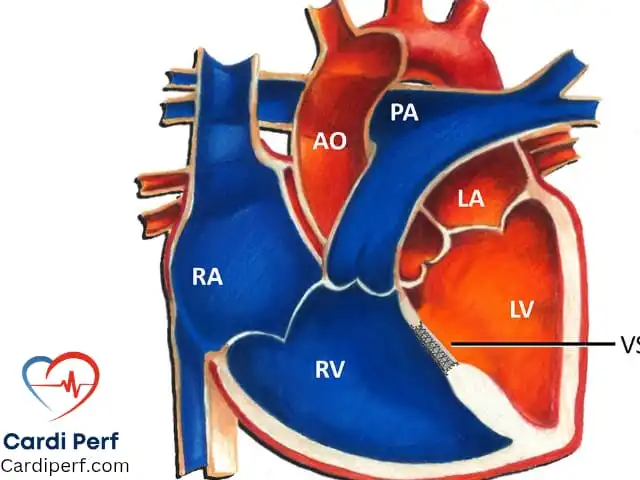
2. Understanding Acute Coronary Syndrome: A Spectrum of Conditions
ACS is not a single entity but rather a group of conditions sharing a common underlying pathophysiology: disruption of a coronary artery plaque, leading to thrombus formation and reduced blood flow to the myocardium.
2.1 Unstable Angina
Unstable angina is characterized by chest pain that occurs at rest or with minimal exertion, is more frequent or severe than previous angina, or lasts longer than usual. It indicates a high risk of progressing to myocardial infarction.
2.2 Myocardial Infarction (Heart Attack)
Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow to a portion of the heart muscle is completely blocked, causing irreversible damage.
2.2.1 STEMI (ST-Elevation Myocardial Infarction)
STEMI is diagnosed by characteristic ST-segment elevation on an electrocardiogram (ECG), indicating complete occlusion of a coronary artery.
2.2.2 NSTEMI (Non-ST-Elevation Myocardial Infarction)
NSTEMI is diagnosed by elevated cardiac biomarkers in the absence of ST-segment elevation on ECG. It usually indicates a partial blockage of a coronary artery.
3. Deciphering the Symptoms of Acute Coronary Syndrome: Time is Muscle
Recognizing the symptoms of ACS promptly is crucial, as “time is muscle.” Key symptoms include:
- Chest pain or discomfort (often described as pressure, tightness, squeezing, or burning)
- Pain radiating to the arm, shoulder, neck, jaw, or back
- Shortness of breath
- Sweating
- Nausea or vomiting
- Lightheadedness or dizziness
- Anxiety
4. The Crucial Role of Rapid Diagnosis in Acute Coronary Syndrome
Prompt diagnosis is essential for effective ACS management.
4.1 Electrocardiogram (ECG)
The ECG is a cornerstone of ACS diagnosis, helping to identify STEMI, arrhythmias, and other cardiac abnormalities.
4.2 Cardiac Biomarkers
Cardiac biomarkers, such as troponin, are released into the bloodstream when heart muscle is damaged. Elevated levels confirm myocardial infarction.
4.3 Other Diagnostic Tests
Other tests, such as echocardiography and coronary angiography, may be used to further evaluate cardiac structure and function and identify the location and severity of coronary artery blockages.
5. Evidence-Based Treatment Strategies for Acute Coronary Syndrome: Restoring Blood Flow
The primary goal of ACS treatment is to restore blood flow to the affected heart muscle as quickly as possible.
5.1 Immediate Management
Initial management includes oxygen therapy, aspirin, and pain relief.
5.2 Pharmacological Interventions
Antiplatelet medications, anticoagulants, and other medications are used to prevent further clot formation and stabilize the patient.
5.3 Revascularization Procedures
Revascularization procedures aim to restore blood flow to the heart.
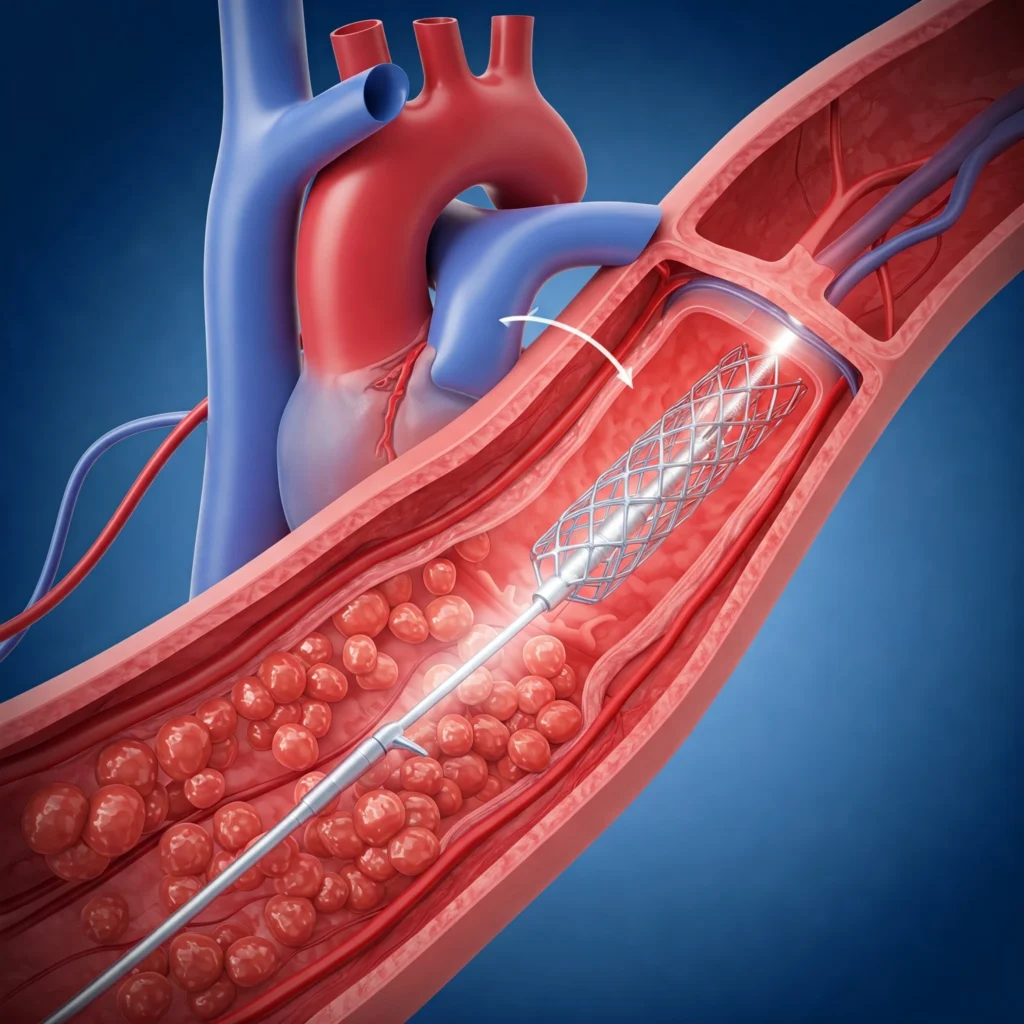
5.3.1 Percutaneous Coronary Intervention (PCI)
PCI involves inserting a catheter into a coronary artery and deploying a stent to open the blockage.
5.3.2 Thrombolytic Therapy
Thrombolytic therapy uses medications to dissolve blood clots.
5.3.3 Coronary Artery Bypass Grafting (CABG)
CABG involves surgically grafting blood vessels to bypass blocked coronary arteries.
6. Risk Factors for Acute Coronary Syndrome: Identifying Vulnerable Individuals
Understanding the risk factors for ACS is crucial for prevention. Key risk factors include:
- Age
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
- Family history of heart disease
- Obesity
- Physical inactivity
7. Empowering Prevention: Reducing the Risk of Acute Coronary Syndrome
Lifestyle modifications and medical management can significantly reduce the risk of ACS.
8. Managing Acute Coronary Syndrome: A Collaborative Approach
Effective ACS management requires a coordinated effort from healthcare professionals across various disciplines.
9. Prognosis and Long-Term Effects of Acute Coronary Syndrome
The prognosis for ACS varies depending on the severity of the event and the timeliness of treatment. Long-term effects can include heart failure, arrhythmias, and recurrent events.
10. Frequently Asked Questions (FAQs) about Acute Coronary Syndrome (ACS)
Here are 10 frequently asked questions about Acute Coronary Syndrome (ACS), complete with answers:
- What are the most common symptoms of Acute Coronary Syndrome? The most common symptom is chest pain or discomfort, often described as pressure, tightness, squeezing, or burning. This pain can radiate to the arm, shoulder, neck, jaw, or back. Other symptoms include shortness of breath, sweating, nausea or vomiting, lightheadedness, and anxiety. It’s crucial to remember that not everyone experiences chest pain; some may have atypical symptoms.
- How is Acute Coronary Syndrome diagnosed? Diagnosis involves several key steps:
- Electrocardiogram (ECG): This is essential for identifying STEMI (ST-elevation myocardial infarction) and other heart rhythm abnormalities.
- Cardiac Biomarkers: Blood tests to measure levels of cardiac enzymes like troponin. Elevated levels indicate heart muscle damage.
- Medical History and Physical Exam: The doctor will ask about your symptoms and medical history.
- Other Tests: Depending on the situation, further tests like echocardiography or coronary angiography may be performed.
- What is the difference between unstable angina and a heart attack (myocardial infarction)? Unstable angina involves chest pain that occurs at rest or with minimal exertion, or that is increasing in frequency or severity. It’s a warning sign. A heart attack (myocardial infarction) occurs when blood flow to a part of the heart is completely blocked, causing heart muscle damage. Heart attacks are categorized as STEMI (ST-elevation myocardial infarction) or NSTEMI (non-ST-elevation myocardial infarction) based on ECG findings.
- What should I do if I think I’m having symptoms of Acute Coronary Syndrome? Call 911 (or your local emergency number) immediately. Do not drive yourself to the hospital. Time is critical in treating ACS, and rapid medical attention can significantly improve outcomes. While waiting for the ambulance, you can chew and swallow an aspirin (if you are not allergic) as directed by the 911 operator.
- What are the risk factors for Acute Coronary Syndrome? The major risk factors include:
- Age (risk increases with age)
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
- Family history of heart disease
- Obesity
- Physical inactivity
- Unhealthy diet
- How can I reduce my risk of Acute Coronary Syndrome? You can reduce your risk by:
- Quitting smoking
- Maintaining a healthy weight
- Eating a heart-healthy diet (low in saturated fat, cholesterol, and sodium)
- Exercising regularly
- Managing high blood pressure, high cholesterol, and diabetes
- Following your doctor’s recommendations for preventive care
- What is the treatment for Acute Coronary Syndrome? Treatment depends on the specific type of ACS and its severity. It often includes:
- Medications (e.g., aspirin, antiplatelet drugs, anticoagulants, nitroglycerin)
- Revascularization procedures (e.g., PCI with stenting, thrombolytic therapy, CABG surgery)
- Lifestyle changes (e.g., diet, exercise, smoking cessation)
- What is a stent? A stent is a small, mesh-like tube that is inserted into a narrowed or blocked coronary artery during PCI. It helps to keep the artery open and restore blood flow to the heart.
- What is the long-term outlook after Acute Coronary Syndrome? The long-term outlook varies depending on the severity of the ACS event, how quickly treatment was received, and overall health. Some people recover fully, while others may experience ongoing heart problems. Cardiac rehabilitation and lifestyle changes are essential for long-term management.
- Is Acute Coronary Syndrome the same as a heart attack? While the terms are often used interchangeably, they aren’t exactly the same. Acute Coronary Syndrome is the overarching term that encompasses a range of conditions, including unstable angina and heart attacks (myocardial infarctions). A heart attack is one type of event within the spectrum of ACS.
11. Conclusion: Advancing ACS Care Through Knowledge and Action
Acute Coronary Syndrome remains a significant public health challenge. By enhancing our understanding of ACS, improving diagnostic accuracy, and implementing timely and effective interventions, healthcare professionals can make a profound difference in the lives of individuals affected by this critical condition. Continued research and education are essential to further advance ACS care and improve patient outcomes. For such detail content about cardiovascular science and perfusion visit us at cardiperf.com
Disclaimer for cardiperf.com
The content on cardiperf.com is intended for healthcare professionals and is provided for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. The information should not be used to diagnose or treat any health condition. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. If you are experiencing a medical emergency, call 911 or your local emergency number immediately.