Table of Contents
- Introduction to Cardiovascular Physiology for Perfusionists
- Understanding Cardiac Output and Stroke Volume
- Hemodynamic Monitoring: Advanced Techniques & Insights
- Blood Pressure Regulation: Impact on Perfusion Science
- Myocardial Oxygen Demand and Oxygen Delivery
- The Significance of Venous Return in Perfusion
- Systemic Vascular Resistance and Its Clinical Implications
- The Role of Preload, Afterload, and Contractility
- Goal-Directed Perfusion (GDP): Precision in Cardiopulmonary Bypass
- 10. Perfusion Strategies for Optimized Patient Outcomes
- Future Trends in Cardiovascular Physiology & Hemodynamic Monitoring
- FAQs: Your Top Questions Answered!
1. Introduction to Cardiovascular Physiology for Perfusionists
👉 Keyword: Cardiovascular physiology, perfusion science
As a perfusionist, mastering cardiovascular physiology is non-negotiable. Whether you’re optimizing hemodynamic parameters during cardiopulmonary bypass (CPB) or monitoring oxygen delivery, understanding these 10 core principles is crucial for advanced patient care.
2. Understanding Cardiac Output and Stroke Volume
👉 Keyword: Cardiac output, stroke volume
- Cardiac Output (CO) = Heart Rate × Stroke Volume
- Stroke Volume (SV) is the amount of blood ejected per heartbeat.
- Why it matters? Maintaining optimal CO ensures effective organ perfusion and oxygen delivery.
🚀 Pro Tip: Advanced perfusion techniques like goal-directed perfusion (GDP) use real-time CO monitoring to optimize outcomes.
3. Key Benefits of Advanced Hemodynamic Monitoring in Cardiac Surgery
👉 Keyword: Hemodynamic monitoring, perfusionist training
Modern hemodynamic monitoring provides real-time insights into cardiac function, vascular resistance, and oxygenation status. Key techniques include:

🔹 Invasive vs. Non-Invasive Hemodynamic Monitoring
- Invasive: Pulmonary artery catheter (Swan-Ganz), arterial line monitoring
- Non-Invasive: Pulse contour analysis, Doppler ultrasound, bioimpedance methods
🔥 Why it’s important: Real-time monitoring enables precise perfusion strategies and prevents organ dysfunction during CPB.
4. Blood Pressure Regulation: Impact on Perfusion Science
👉 Keyword: Blood pressure regulation, systemic vascular resistance
Blood pressure (BP) is a critical perfusion parameter influenced by:
- Systemic Vascular Resistance (SVR)
- Cardiac Output (CO)
- Blood Volume & Viscosity
🩸 Clinical Insight: During CPB, maintaining mean arterial pressure (MAP) between 50-80 mmHg ensures optimal perfusion.
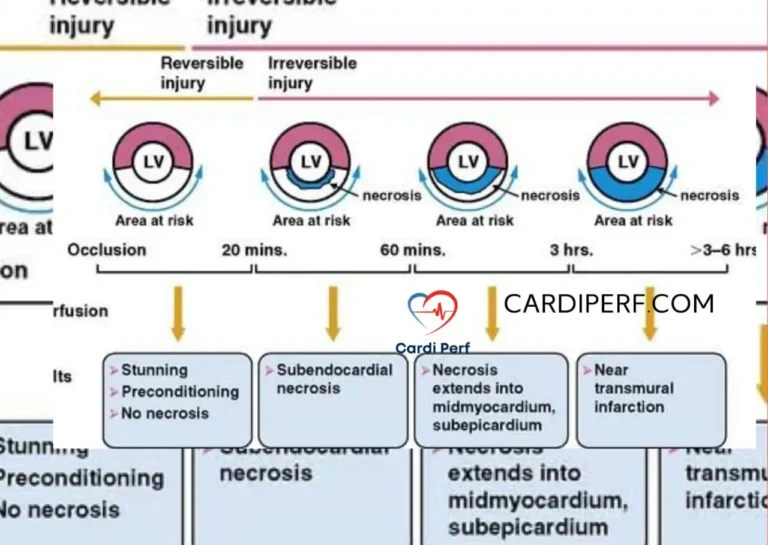
5. Myocardial Oxygen Demand and Oxygen Delivery
👉 Keyword: Myocardial oxygen demand, oxygen delivery
- Oxygen Delivery (DO2) depends on cardiac output and arterial oxygen content.
- Oxygen Consumption (VO2) reflects metabolic demand.
- The DO2/VO2 ratio must remain optimal to prevent anaerobic metabolism and acidosis.
💡 Pro Tip: Maintaining optimal hematocrit levels (24-30%) during CPB enhances oxygen delivery without increasing viscosity.
6. The Significance of Venous Return in Perfusion
👉 Keyword: Venous return, perfusion strategies
Venous return is vital for cardiac preload and is influenced by:
- Central Venous Pressure (CVP)
- Blood volume status
- Respiratory mechanics
🚑 Clinical Tip: Adjusting venous reservoir levels prevents hypovolemia and venous air embolism during CPB.
7. Systemic Vascular Resistance and Its Clinical Implications
👉 Keyword: Systemic vascular resistance, perfusionist training
- SVR is the resistance blood faces as it moves through circulation.
- High SVR = Increased afterload → Higher myocardial oxygen demand
- Low SVR = Hypotension → Risk of organ hypoperfusion
🩺 Perfusion Strategy: Balance SVR with vasoactive agents (e.g., norepinephrine, vasodilators).
8. The Role of Preload, Afterload, and Contractility
👉 Keyword: Preload, afterload, cardiac contractility
Preload: The end-diastolic volume determining myocardial stretch.
Afterload: The resistance against which the heart pumps.
Contractility: The inotropic state of the myocardium.
🎯 Key Clinical Insight: Excessive preload increases LVEDP, leading to pulmonary congestion and low cardiac output syndrome (LCOS) postoperatively.
9. The Role of Goal-Directed Perfusion in Optimizing Oxygen Delivery
👉 Keyword: Goal-directed perfusion, perfusion strategies, hemodynamic monitoring
What is Goal-Directed Perfusion (GDP)?
Goal-Directed Perfusion (GDP) is a patient-specific, evidence-based strategy that optimizes perfusion parameters during cardiopulmonary bypass (CPB). Instead of relying on fixed blood flow rates, GDP dynamically adjusts perfusion based on real-time physiological needs. Hemodynamic management in cardiac surgery
🔹 Core Objectives of GDP in Perfusion Science
- Maintain Optimal Oxygen Delivery (DO₂): Prevents ischemia and anaerobic metabolism.
- Regulate Perfusion Pressure (MAP): Ensures adequate organ perfusion.
- Prevent Hemodilution & Inflammatory Response: Reduces complications post-CPB.
- Monitor & Adjust Hemodynamic Parameters in Real-Time: Uses advanced sensors, near-infrared spectroscopy (NIRS), and continuous CO₂ monitoring.
🔹 Key Parameters Used in GDP
- Oxygen Delivery Index (DO₂i): ≥280-300 mL/min/m² recommended.
- Mean Arterial Pressure (MAP): 60-80 mmHg.
- Hematocrit (Hct): Maintained between 24-30% to optimize oxygen transport.
- Lactate Levels: Used as a marker for tissue perfusion efficiency.
- pH & Acid-Base Balance: Metabolic acidosis is a red flag for inadequate perfusion.

🔹 Technologies Driving GDP Implementation
🚀 Artificial Intelligence (AI) & Machine Learning → AI-assisted GDP is being used to predict patient-specific oxygen needs and adjust perfusion in real-time.
🔬 Advanced Hemodynamic Monitors → Newer perfusion devices now integrate real-time blood gas analyzers and tissue perfusion sensors.
🩸 Point-of-Care Testing (POCT) → Continuous lactate, SvO₂, and microcirculation monitoring enhance GDP precision.
Why Every Perfusionist Should Adopt GDP?
✅ Lower Postoperative Complications: Reduces risks of AKI (Acute Kidney Injury), stroke, and cognitive dysfunction.
✅ Improved Patient Outcomes: Personalized perfusion leads to faster recovery and reduced ICU stay.
✅ Evidence-Based & Future-Proof: Backed by extensive clinical studies in perfusion science.
🔥 Takeaway: If you’re not using Goal-Directed Perfusion, you’re missing out on the future of perfusion science!
10. Perfusion Strategies for Optimized Patient Outcomes
👉 Keyword: Perfusion strategies, hemodynamic monitoring
- Goal-Directed Perfusion (GDP)
- Personalized Blood Flow Adjustments
- Optimizing Oxygenation & Acid-Base Balance
📌 New Trends: AI-driven perfusion software is improving precision in blood flow regulation.
11. Future Trends in Cardiovascular Physiology & Hemodynamic Monitoring
👉 Keyword: Future trends in perfusion, advanced hemodynamic monitoring
🔹 Artificial Intelligence (AI) in Perfusion
🔹 Automated Hemodynamic Monitoring Systems
🔹 Real-Time Oxygenation & Tissue Perfusion Mapping
🚀 Takeaway: The future of perfusion science is data-driven and AI-enhanced, ensuring better patient outcomes!

11. FAQs: Your Top Questions Answered! ✅
1. What is the most critical cardiovascular parameter for a perfusionist?
Cardiac output (CO) and oxygen delivery (DO₂) are the most critical factors. Maintaining a high DO₂ index (≥280 mL/min/m²) during CPB is key to avoiding tissue hypoxia.
2. What is the ideal MAP during cardiopulmonary bypass?
The optimal mean arterial pressure (MAP) during CPB is 60-80 mmHg to ensure adequate perfusion without excessive afterload on the heart.
3. Why is venous return crucial in perfusion?
Venous return determines preload, directly impacting stroke volume and cardiac output. Poor venous return can lead to hypoperfusion and metabolic acidosis.
4. How does systemic vascular resistance (SVR) affect perfusion?
- High SVR = Increased afterload → Higher myocardial oxygen demand.
- Low SVR = Hypotension → Risk of organ hypoperfusion.
Balancing SVR is key to optimal circulation!
5. What is the significance of lactate monitoring in perfusion?
High lactate levels (>2.0 mmol/L) indicate anaerobic metabolism and inadequate tissue oxygenation, signaling poor perfusion during CPB.
6. What is Goal-Directed Perfusion (GDP) in simple terms?
GDP is a precision-based perfusion strategy that adjusts blood flow, pressure, and oxygenation in real time based on the patient’s physiological needs.
7. How does perfusion affect postoperative recovery?
Poor perfusion during CPB increases the risk of acute kidney injury (AKI), neurocognitive decline, and systemic inflammatory response syndrome (SIRS), leading to longer ICU stays.
8. What role does hematocrit (Hct) play in perfusion?
Maintaining hematocrit levels between 24-30% optimizes oxygen transport and viscosity, preventing excessive hemodilution.
9. What are the latest technologies in hemodynamic monitoring?
- AI-powered perfusion software
- Real-time cerebral oximetry (NIRS)
- Continuous non-invasive cardiac output (NICOM)
These technologies are revolutionizing precision perfusion!
10. What’s the biggest mistake a perfusionist can make?
🚨 Ignoring Goal-Directed Perfusion principles! Sticking to fixed flow rates instead of using real-time hemodynamic data can lead to hypoperfusion, tissue ischemia, and organ failure.
Conclusion
Understanding cardiovascular physiology is non-negotiable for perfusionists. Implementing Goal-Directed Perfusion (GDP) and using advanced hemodynamic monitoring ensures precision, safety, and better patient outcomes.
📢 Did this guide help you? Share it with your perfusion colleagues! 🚀
Conclusion
Mastering cardiovascular physiology is essential for perfusionists to optimize hemodynamics, oxygen delivery, and patient safety. Staying updated with advanced monitoring techniques ensures precision and efficiency in perfusion science.
📢 Share this with your perfusion colleagues & stay ahead in the field! 🚀for latest update visit us at cardiperf.com