Vacuum-assisted venous drainage (VAVD) has emerged as an indispensable tool in cardiopulmonary bypass (CPB), particularly in minimally invasive and complex cardiac surgeries. By optimizing venous return, reducing circuit prime volume, and improving overall surgical outcomes, VAVD has revolutionized the way perfusionists and surgical teams approach CPB. However, its safe and effective application demands strict adherence to updated guidelines and best practices.
The European Association for Cardiothoracic Surgery (EACTS) and the European Board of Cardiovascular Perfusion (EBCP) have recently released critical updates to ensure the safe integration of VAVD into CPB protocols. Additionally, organizations like AmSECT and Perfusion.com provide standardized operating procedures (SOPs) to guide its use. As technology continues to advance, staying aligned with these evolving standards is essential to safeguard patient safety while maximizing the benefits of VAVD.
Understanding VAVD: A Game-Changer in Cardiopulmonary Bypass
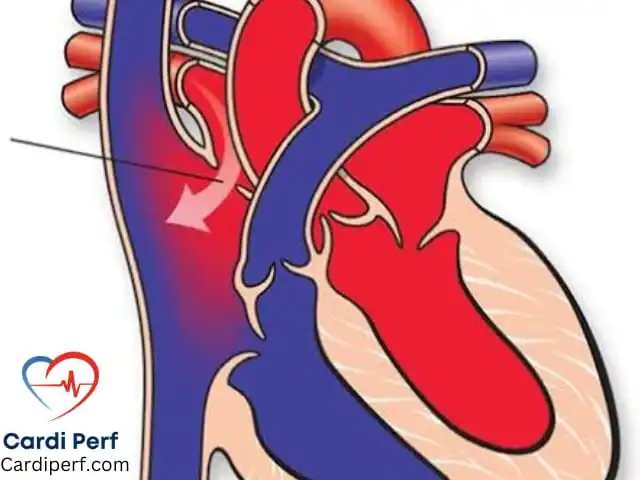
Vacuum-assisted venous drainage (VAVD) has become a cornerstone of modern CPB systems, particularly in procedures requiring minimally invasive approaches or involving complex anatomical challenges. Unlike traditional gravity-dependent venous drainage, VAVD uses controlled vacuum pressure to enhance venous return to the heart-lung machine. This innovation not only improves the efficiency of blood flow but also addresses many of the limitations associated with conventional methods.
Why VAVD Matters in Modern Cardiac Surgery
In minimally invasive cardiac surgeries, where access to the heart is limited, achieving optimal venous drainage can be challenging. VAVD overcomes this by providing consistent and reliable venous return, even in low-flow scenarios. This capability is particularly valuable in surgeries such as robotic-assisted mitral valve repairs, transcatheter aortic valve replacements (TAVR), and other procedures that require smaller incisions and reduced surgical trauma.
Additionally, VAVD plays a pivotal role in reducing circuit prime volume—a key factor in minimizing hemodilution during CPB. Hemodilution can lead to complications such as anemia, coagulopathy, and increased transfusion requirements. By lowering the amount of fluid needed to prime the CPB circuit, VAVD helps maintain higher hematocrit levels, improving oxygen delivery and reducing postoperative complications.
Key Benefits of VAVD in CPB
The adoption of VAVD has brought about significant improvements in both surgical efficiency and patient outcomes. Below are some of the most notable benefits:
1. Enhanced Venous Drainage Efficiency
VAVD ensures consistent and reliable venous return, even in challenging surgical scenarios. This stability allows perfusionists to maintain optimal flow rates, reducing the risk of air entrainment and ensuring uninterrupted support during CPB.
2. Reduced Circuit Prime Volume
One of the standout advantages of VAVD is its ability to minimize circuit prime volume. Lower prime volumes translate to reduced hemodilution, which is directly linked to improved patient outcomes. Studies have shown that patients undergoing CPB with VAVD experience fewer transfusions, lower rates of postoperative complications, and faster recovery times.
3. Improved Outcomes in Minimally Invasive Surgeries
Minimally invasive cardiac surgeries rely heavily on advanced technologies like VAVD to compensate for limited access and reduced surgical space. By optimizing venous drainage, VAVD enables surgeons to perform intricate procedures with greater precision and confidence, ultimately leading to better results for patients.
4. Flexibility in Surgical Approaches
VAVD’s versatility makes it suitable for a wide range of cardiac procedures, from routine coronary artery bypass grafting (CABG) to highly complex congenital heart defect repairs. Its adaptability ensures that surgical teams can tailor their approach to each patient’s unique needs, enhancing both safety and effectiveness.
Pros and Cons of Using VAVD in CPB
While VAVD offers numerous advantages, it is important to weigh its pros and cons to ensure safe and effective implementation.
Pros of VAVD
- Improved Venous Return: Ensures consistent and reliable blood flow, even in low-flow scenarios.
- Reduced Hemodilution: Lowers circuit prime volume, maintaining higher hematocrit levels and improving oxygen delivery.
- Enhanced Surgical Precision: Supports minimally invasive techniques, enabling surgeons to perform complex procedures with greater accuracy.
- Versatility: Suitable for a wide range of cardiac surgeries, including pediatric and adult cases.
- Faster Recovery Times: Patients experience fewer complications and shorter hospital stays due to optimized CPB conditions.
Cons of VAVD
- Risk of Air Embolism: Excessive negative pressure can introduce air into the venous lines, posing a serious risk to patients.
- Hemodynamic Instability: High vacuum levels may cause fluctuations in blood pressure, particularly in frail or pediatric patients.
- Equipment Malfunction: Mechanical issues, such as line occlusion or pump failure, can disrupt the procedure.
- Learning Curve: Proper setup and monitoring require specialized training, which may be challenging for new practitioners.
- Cost Implications: Advanced VAVD systems and maintenance can be expensive, potentially limiting accessibility in resource-constrained settings.
Updated Guidelines for Safe VAVD Use:
To ensure the safe and effective use of VAVD, several organizations have published comprehensive guidelines. Below is a summary of key recommendations from EACTS , EBCP , AmSECT , and Perfusion.com .
1. Equipment Setup and Calibration
- Vacuum levels should be calibrated based on patient-specific factors, including body size, venous anatomy, and surgical requirements. All components of the VAVD system must undergo rigorous preoperative testing.
- Recommend using vacuum regulators with precise control mechanisms and ensuring all connections are secure and airtight.
- Emphasize the importance of using high-quality tubing and filters to prevent air entrainment and maintain optimal flow dynamics.
2. Continuous Monitoring During CPB
- EACTS/EBCP Guidelines: Real-time monitoring of vacuum pressure, flow rates, and potential issues such as air entrainment or line occlusion is mandatory.
- AmSECT SOPs: Suggest integrating advanced monitoring systems that provide instant feedback and alarms for abnormal conditions.
- Perfusion.com Guidelines: Advocate for regular checks of hemodynamic parameters, including central venous pressure (CVP) and arterial pressure, to ensure stability.
3. Troubleshooting Protocols
- EACTS/EBCP Guidelines: Outline standardized protocols for addressing common issues, such as sudden drops in venous return or unexpected increases in vacuum pressure.
- AmSECT SOPs: Provide step-by-step instructions for troubleshooting equipment malfunctions, including backup plans for emergencies.
- Perfusion.com Guidelines: Stress the importance of having a dedicated team member responsible for monitoring and adjusting VAVD settings throughout the procedure.
4. Training and Education
- Recommend regular workshops, simulations, and certification programs to keep practitioners updated on the latest advancements.
- Offer online courses and hands-on training sessions focused on VAVD setup, operation, and troubleshooting.
- Encourage participation in professional conferences and webinars to stay informed about emerging trends and technologies.

Challenges and Considerations in VAVD Application
While VAVD offers significant advantages, its implementation is not without challenges. Addressing these concerns is essential to maximizing the benefits of VAVD while safeguarding patient safety.
Risk of Air Embolism
One of the primary risks associated with VAVD is the potential for air embolism, which can occur if excessive negative pressure causes air to enter the venous lines. To mitigate this risk, surgical teams must carefully monitor vacuum levels and ensure that all connections are secure and airtight.
Hemodynamic Instability
Excessive vacuum pressure can lead to hemodynamic instability, particularly in pediatric or frail patients. The updated guidelines stress the importance of tailoring vacuum levels to individual patient characteristics and continuously monitoring hemodynamic parameters throughout the procedure.
Equipment Malfunction
Like any mechanical system, VAVD equipment is susceptible to malfunctions. Regular maintenance, preoperative checks, and backup plans are essential to addressing potential issues promptly and minimizing disruptions during surgery.
The Future of VAVD in Cardiac Surgery
As technology continues to advance, the role of VAVD in CPB is expected to expand further. Innovations in materials, sensors, and automation are paving the way for smarter, more efficient VAVD systems. For example, next-generation devices may incorporate AI-driven algorithms to predict and prevent complications in real time, enhancing both safety and performance.
Integration with Smart Monitoring Systems
Future VAVD systems are likely to integrate seamlessly with smart monitoring platforms, providing real-time data analytics and predictive insights. These capabilities will enable perfusionists to anticipate and address potential issues before they escalate, further improving patient outcomes.
Customization for Individual Patients
Advances in personalized medicine are driving the development of customizable VAVD solutions tailored to individual patient needs. From adjustable vacuum levels to patient-specific circuit designs, these innovations will allow surgical teams to optimize CPB protocols for every case.
Broader Applications in Non-Cardiac Procedures
While VAVD is primarily used in cardiac surgery, its applications are expanding to other fields, such as organ transplantation and extracorporeal membrane oxygenation (ECMO). As these technologies mature, VAVD is poised to play an increasingly vital role in a wide range of medical procedures.
Embracing VAVD: A Call to Action for Healthcare Providers
The integration of VAVD into CPB represents a significant advancement in cardiac surgery, offering unparalleled benefits in terms of efficiency, safety, and patient outcomes. For perfusionists, students, and healthcare providers, staying informed about the latest developments and adhering to updated guidelines is essential to harnessing the full potential of this technology.
To ensure safe and effective use of VAVD, healthcare organizations should prioritize staff training, invest in high-quality equipment, and establish robust quality assurance protocols. Collaboration with industry partners and participation in professional organizations like EACTS, EBCP, AmSECT, and Perfusion.com can also help keep teams at the forefront of innovation.
By embracing VAVD and aligning with evolving standards, healthcare providers can continue to deliver exceptional care and drive positive outcomes for their patients. Visit CardiPerf.com today to learn more about how VAVD and other advancements in perfusion technology are shaping the future of cardiac surgery.
Frequently Asked Questions (FAQs)
1. What is vacuum-assisted venous drainage (VAVD)?
VAVD is a technique used during cardiopulmonary bypass (CPB) to enhance venous return using controlled vacuum pressure. It improves efficiency and reduces circuit prime volume, making it ideal for minimally invasive and complex surgeries.
2. How does VAVD improve patient outcomes?
VAVD reduces hemodilution, lowers transfusion requirements, and enhances surgical precision, leading to faster recovery times and fewer complications.
3. What are the risks of using VAVD?
Potential risks include air embolism, hemodynamic instability, and equipment malfunction. Proper setup, monitoring, and adherence to guidelines minimize these risks.
4. What do the updated EACTS guidelines recommend for VAVD?
The guidelines emphasize proper equipment calibration, continuous monitoring, standardized troubleshooting protocols, and ongoing training for healthcare providers.
5. Can VAVD be used in pediatric surgeries?
Yes, VAVD can be used in pediatric cases, but vacuum levels must be carefully adjusted to accommodate smaller patients and prevent hemodynamic instability.
6. How does VAVD support minimally invasive surgeries?
VAVD optimizes venous drainage in limited-access scenarios, enabling surgeons to perform complex procedures with greater precision and confidence.
7. What is the future of VAVD technology?
Future innovations may include AI-driven monitoring, customizable solutions, and broader applications in non-cardiac procedures.
8. How can perfusionists stay updated on VAVD advancements?
Perfusionists should participate in workshops, certifications, and professional organizations like EACTS, EBCP, AmSECT, and Perfusion.com to stay informed about the latest developments.
9. Is VAVD suitable for all cardiac surgeries?
While VAVD is highly versatile, its application depends on patient-specific factors and surgical requirements. A thorough assessment is necessary for each case.
10. Where can I learn more about VAVD and CPB?
Visit CardiPerf.com for resources, articles, and updates on VAVD and other advancements in perfusion technology.