Cardiac surgery relies heavily on cardiopulmonary bypass (CPB) to maintain circulation and oxygenation while the heart is stopped. However, hypoxia during CPB is a critical complication that can lead to severe consequences if not promptly recognized and managed. In this article, we discuss the causes, diagnostic approach, and solutions for hypoxia on bypass to help perfusionists and cardiac surgeons navigate this challenging scenario.
Understanding Hypoxia on Cardiopulmonary Bypass
Hypoxia on bypass is defined as a drop in arterial oxygen saturation (SaO₂) below acceptable levels, typically below 95%. A gradual decrease in oxygen saturation despite full flow settings indicates a systemic issue with oxygenation that requires immediate attention. Hypoxia can lead to multiple complications, including end-organ damage, acidosis, and cardiac arrest, necessitating immediate corrective action.
Common Causes of Hypoxia on Bypass
1. Oxygen Supply Issues
- Disconnection of the oxygen line to the oxygenator
- Depleted oxygen supply in the gas source (empty oxygen tank)
- Kinked or obstructed gas lines
- Malfunctioning gas blender delivering inadequate FiO₂
- Incorrect gas mixtures leading to hypoxic gas delivery
2. Oxygenator Dysfunction
- Failure of the membrane oxygenator due to clot formation or fibrin deposition
- Gas transfer impairment from protein or fat embolization
- Increased CO₂ retention due to inadequate sweep gas flow
- Water-to-blood leakage leading to oxygenator flooding
- Silicone membrane degradation reducing gas exchange efficiency
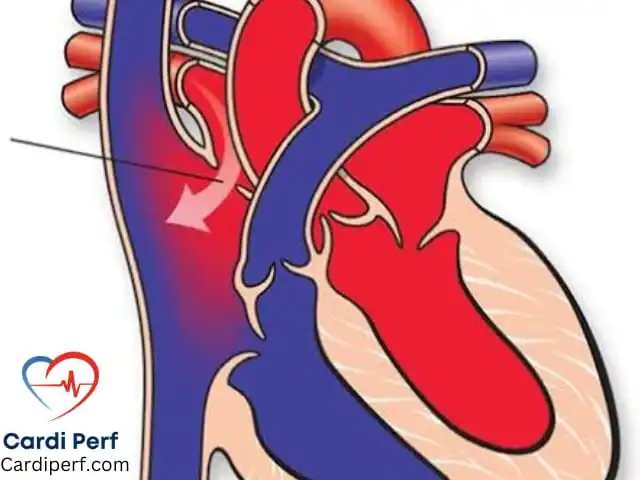
3. Maldistribution of Blood Flow
- Malpositioned venous or arterial cannula
- Significant recirculation due to improper cannula positioning
- Excessive blood shunting through an intra-cardiac defect
- Differential hypoxia in femoral cannulation due to inadequate upper-body perfusion
4. Ventilation Problems (If the Heart is Beating)
- Inadequate lung ventilation in cases of partial bypass
- Atelectasis due to prolonged non-ventilation
- Pulmonary edema secondary to fluid overload or inadequate LV venting
- High pulmonary vascular resistance affecting oxygen uptake
Step-By-Step Troubleshooting Approach
When faced with dropping SaO₂ on bypass, a structured approach is essential:
1. Verify Oxygenation of the Circuit
- Check the color of arterial and venous blood:
- Bright red = oxygenation is working
- Dark = impaired oxygenation
- Ensure the gas line is connected and functional
- Confirm the FiO₂ setting is at 100%
- Check the sweep gas flow to confirm CO₂ clearance
- Inspect the oxygenator for signs of flooding or malfunction
2. Assess Oxygenator Performance
- Review the pre- and post-membrane blood gases
- If PaO₂ remains low despite 100% FiO₂, suspect oxygenator failure
- Consider an oxygenator change if function does not improve
- Increase gas flow rates to assess responsiveness
3. Rule Out Mechanical and Cannulation Issues
- Verify venous drainage to avoid venous air entrainment
- Assess arterial cannula placement to ensure proper distribution
- Perform a TEE (transesophageal echocardiogram) to detect intracardiac shunting
- Check for excessive line pressures that may indicate blockages
4. Address Ventilation and Perfusion Mismatches
- If the heart is still ejecting, ensure the lungs are ventilated
- Check for pulmonary embolism, atelectasis, or severe pulmonary hypertension
- Consider increasing FiO₂ and applying lung recruitment maneuvers
- Assess for right ventricular dysfunction affecting pulmonary circulation
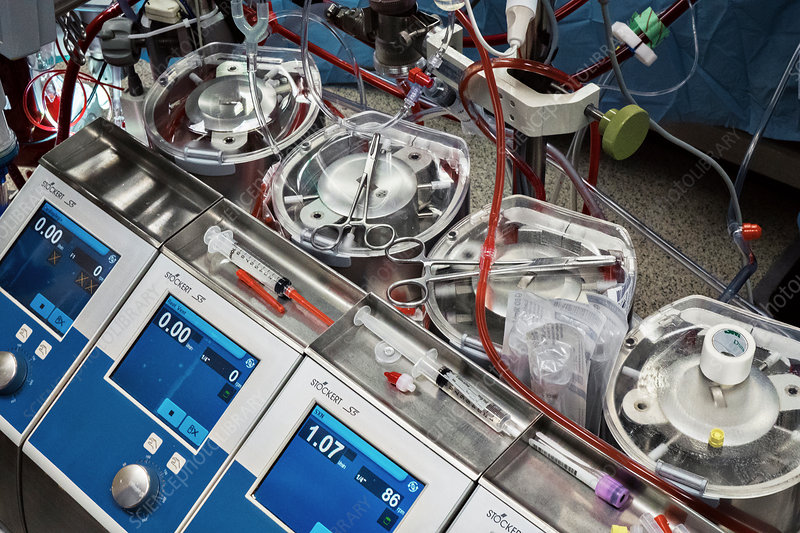
Management of Oxygenator Failure: When to Exchange
If increasing FiO₂ and sweep gas does not improve oxygenation, an oxygenator exchange may be required.
Steps for Safe Oxygenator Exchange
- Ensure a backup oxygenator is available
- Clamp arterial and venous lines to the patient
- Clamp inflow, outflow, cardioplegia, and recirculation lines
- Replace the oxygenator and reattach all connections
- De-air the circuit before resuming bypass flow
- Perform blood gas analysis post-exchange to confirm oxygenation improvement
Advanced Monitoring for Hypoxia Prevention
1. Continuous Near-Infrared Spectroscopy (NIRS)
- Provides real-time regional cerebral oxygen saturation
- Helps detect inadequate perfusion before SaO₂ drops
2. Transcutaneous Oxygen Monitoring
- Measures oxygen tension in peripheral tissues
- Early indicator of systemic hypoxia before organ dysfunction
3. Inline Blood Gas Monitoring
- Allows real-time assessment of PaO₂, PCO₂, and pH
- Helps detect oxygenator failure before clinical deterioration
4. Perfusion Index (PI) and Oxygen Extraction Ratio (OER)
- Assesses global perfusion adequacy
- Guides interventions to optimize oxygen delivery
Preventing Hypoxia on Bypass: Key Takeaways
- Pre-Bypass Checklist: Always verify oxygen supply and gas connections before starting CPB.
- Situational Awareness: Monitor real-time perfusion parameters and blood gases.
- Rapid Communication: Empower the OR team to speak up about any unexpected drops in SaO₂.
- Backup Plan: Always have a secondary oxygenator and gas supply ready.
- Routine Maintenance: Regularly check gas blenders, oxygenators, and gas supply systems.
- Simulation Drills: Conduct mock hypoxia scenarios to enhance crisis response.
- Early Warning Systems: Utilize continuous monitoring technologies for early detection.
FAQs About Hypoxia on Bypass
- What is the most common cause of hypoxia on bypass?
- Oxygen supply disconnection or failure is the most frequent issue.
- How can you quickly diagnose oxygenator failure?
- Check pre- and post-membrane blood gases; low PaO₂ despite 100% FiO₂ suggests failure.
- Can a hypoxic patient be ventilated while on bypass?
- If partial bypass is used, ventilation should continue for oxygen delivery.
- How often should oxygenator performance be checked?
- Blood gases should be analyzed frequently to monitor oxygenation efficiency.
- What is the role of TEE in troubleshooting hypoxia?
- TEE helps detect cannulation issues and intracardiac shunting.
- Can an oxygenator be exchanged while on full bypass?
- Yes, using safe clamping and de-airing techniques.
- What early signs suggest an impending oxygenation issue?
- Gradual PaO₂ decline, rising PCO₂, and darker arterial blood color.
- How can perfusionists prepare for oxygenator failure?
- Always have a backup oxygenator and a predefined exchange plan.
- Does increasing FiO₂ always fix hypoxia on bypass?
- No, if the oxygenator is failing, FiO₂ adjustments won’t help.
- What are the risks of prolonged hypoxia on bypass?
- End-organ damage, acidosis, and potential cardiac arrest.
For more expert insights on perfusion science and cardiac surgery, stay tuned to CardiPerf.com—your go-to resource for cutting-edge advancements in perfusion and ECMO technology.