CPB Technology and Techniques Examination
Comprehensive MCQ Examination – 100 Questions
CPB Circuit Components
Comprehensive coverage of CPB circuit components, oxygenators, pumps, and physiological principles.
CPB Techniques & Management
Clinical applications, cannulation strategies, myocardial protection, and hemodynamic management.
Exam Structure – 100 Questions
Important Instructions
- Each question has a 45-second time limit
- You cannot go back to previous questions once answered
- The exam will automatically submit when time expires
- You need a score of 75% or higher to pass
- All questions are based on established CPB guidelines and standards
Cardiopulmonary Bypass (CPB) is the backbone of modern cardiac surgery. If surgery is the art, CPB Technology and Techniques are the science that keeps the patient alive while the heart sleeps. For perfusionists, CPB is not just equipment—it’s physiology in motion, real-time decision-making, and razor-sharp precision under pressure.
This guide is built exclusively for the cardiac surgery team—especially perfusionists, combining clinical practicality with future-ready knowledge. From circuit design to oxygenation science, anticoagulation, monitoring, safety systems, and next-gen automation, this is your all-in-one CPB mastery blueprint.
What Is Cardiopulmonary Bypass (CPB)? – A Physiological Perspective
Cardiopulmonary Bypass is a mechanical system that temporarily replaces heart and lung function during open-heart surgery. It maintains:
- Systemic perfusion
- Gas exchange (oxygenation and CO₂ removal)
- Temperature control
- Acid–base and electrolyte balance
Core Physiologic Functions of CPB
- Oxygen delivery (DO₂)
- Carbon dioxide elimination
- Hemodynamic support
- Thermal regulation
- Blood conservation
Without optimized CPB Technology and Techniques, complex cardiac surgery would be impossible.
Evolution of CPB Technology – From Roller Pumps to Smart Automation
CPB systems have evolved from bulky mechanical circuits to precision-controlled digital platforms.
First-Generation CPB
- Roller pumps
- Bubble oxygenators
- Gravity venous drainage
- High hemodilution and inflammatory response
Modern CPB Systems
- Centrifugal pumps
- Hollow-fiber membrane oxygenators
- Integrated arterial filters
- Biocompatible coatings
- Servo-controlled safety systems
Current Focus of CPB Innovation
- Reduced blood–surface interaction
- Miniaturized circuits (MiECC)
- Microemboli detection
- Automation and AI-guided perfusion
The future of CPB Technology and Techniques is moving toward closed-loop intelligent perfusion.
Essential Components of the Modern CPB Circuit
Understanding every component of the CPB circuit is non-negotiable for perfusionists.
Venous Drainage System
- Gravity drainage
- VAVD (Vacuum Assisted Venous Drainage)
- Kinetic venous drainage
Maintains preload and prevents venous hypertension.
Venous Reservoir
- Open vs closed systems
- Air handling capability
- Volume buffering during fluctuations
Blood Pump Technology
- Roller Pumps: Fixed displacement, higher hemolysis risk
- Centrifugal Pumps: Pressure-dependent, safer for pediatric and adult CPB
Centrifugals now dominate modern CPB Technology and Techniques due to lower trauma.
Oxygenators – The Artificial Lung
- Hollow fiber membrane oxygenators
- Integrated heat exchangers
- Low-prime pediatric designs
Key Oxygenator Performance Parameters
- Rated flow
- Pressure drop
- Heat exchange efficiency
- Plasma leakage resistance
Arterial Line Filtering
- Removes microemboli
- Reduces neurological complications
- Standard pore size: 40 µm
Heat Exchanger
- Systemic temperature management
- Enables hypothermia and rewarming protocols
CPB Anticoagulation and ACT Management
No CPB technology works without safe anticoagulation.
Heparin Dosing Strategies
- Weight-based
- Concentration-based
- Heparin dose-response curves
Activated Clotting Time (ACT)
- Target: > 400–480 seconds
- Pediatric CPB often requires higher thresholds
Protamine Reversal
- Heparin-protamine ratio
- Risk of hypotension, pulmonary hypertension
ACT control is a cornerstone of safe CPB Technology and Techniques.
CPB Perfusion Flow Dynamics and Indexed Parameters
Pump Flow Calculation
- Based on Body Surface Area (BSA)
- Standard adult CI: 2.2–2.6 L/min/m²
Mean Arterial Pressure (MAP) Targets
- Adults: 50–70 mmHg
- Pediatrics: 30–50 mmHg
Systemic Vascular Resistance (SVR)
SVR guides:
- Vasoconstrictor use
- Flow adjustments
- Microcirculatory optimization
CPB Gas Exchange Technology and Sweep Control
Oxygenation Control
- FiO₂ regulation
- Oxygen transfer capacity
- Hemoglobin-dependent DO₂
Carbon Dioxide Removal
- Sweep gas flow
- Membrane efficiency
- Blood flow coupling
Alpha-Stat vs pH-Stat Management
- Adult normothermia favors alpha-stat
- Pediatric hypothermia favors pH-stat
Advanced CPB Technology and Techniques demand real-time ABG-driven gas control.
Hemodilution, Ultrafiltration, and Blood Conservation
Hemodilution Effects
- Reduced oxygen-carrying capacity
- Decreased oncotic pressure
- Increased edema risk
Conventional Ultrafiltration (CUF)
- Performed during CPB
- Removes plasma water
- Concentrates RBCs
Modified Ultrafiltration (MUF)
- Performed post-CPB
- Essential in pediatric cardiac surgery
- Improves ventricular performance and oxygenation
Cell Saver Integration
- Reduces allogeneic transfusion
- Preserves autologous RBCs
- Key blood management tool
Blood conservation is a defining pillar of elite CPB Technology and Techniques.
Inflammatory Response and Biocompatibility in CPB
CPB activates:
- Complement cascade
- Leukocytes
- Cytokine storm
Modern Circuit Coatings
- Heparin-bonded
- Phosphorylcholine
- Albumin coatings
These reduce:
- SIRS
- Coagulopathy
- Post-operative organ dysfunction
Neuromonitoring and Organ Protection on CPB
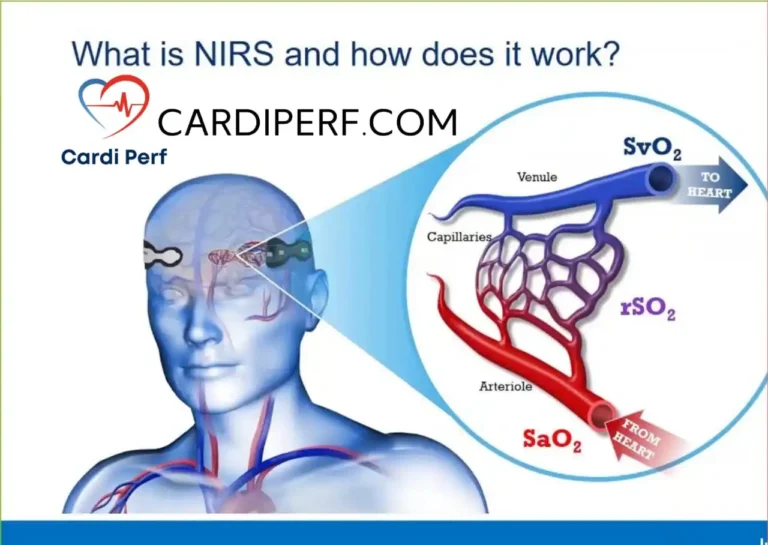
Cerebral Oximetry (NIRS)
- Real-time brain oxygenation
- Detects low flow states
- Guides perfusion optimization
Renal Protection Strategies
- Adequate MAP
- Pulsatile perfusion
- Avoidance of excessive hemodilution
Pediatric vs Adult CPB Technology
Pediatric CPB Challenges
- Small blood volume
- High hemodilution risk
- Immature organ systems
Specialized Pediatric CPB Solutions
- Low-prime oxygenators
- Micro-circuits
- MUF protocols
- Precision flow control
Pediatric CPB Technology and Techniques demand absolute accuracy—no margin for error.
Safety Systems and Incident Prevention in CPB
Air Detection Systems
- Ultrasonic bubble detectors
- Automated pump stop
Pressure Monitoring
- Pre- and post-oxygenator
- Arterial line pressure
- Venous line pressure
Temperature Micro-Control
- Prevents gaseous embolism
- Controls rewarming gradients
Digital Integration and Smart Perfusion Platforms
Modern CPB is now data-driven.
Integrated Data Recording
- Flow
- Pressures
- Gases
- Temperature
Closed-Loop Perfusion Systems
- Automatic flow control
- AI-assisted oxygen targeting
- Predictive alarm systems
This is the future of CPB Technology and Techniques—perfusion augmented by intelligence.
ECMO vs CPB – Technology Overlap and Key Differences
| Parameter | CPB | ECMO |
|---|---|---|
| Duration | Hours | Days to weeks |
| Anticoagulation | High ACT | Lower sustained |
| Circuit Type | Open | Closed |
| Oxygenation | Full support | Partial/Full |
The technological principles overlap, but CPB Technology and Techniques prioritize short-term high-intensity support.
Common CPB Complications and Perfusionist Counter-Strategies
Air Embolism
- Prevention with filters and vigilance
Hemolysis
- Avoid excessive negative pressure
- Use centrifugal pumps
Low Flow States
- Monitor DO₂, lactate, venous saturation
Coagulopathy
- ACT optimization
- Ultrafiltration balance
Perfusionists don’t just run machines—we prevent disasters before they happen.
The Future of CPB Technology – Where We’re Headed
The next decade of CPB Technology and Techniques is wild—in the best way.
Emerging Innovations
- Miniaturized fully closed CPB
- AI-guided perfusion algorithms
- Smart oxygenators with real-time sensors
- Robotic perfusion integration
- Personalized perfusion protocols
Perfusion science is shifting from operator-dependent to intelligence-assisted precision medicine. And yes—perfusionists are leading this revolution.
Why Perfusionist Mastery of CPB Technology Is Non-Negotiable
You are not just “running a machine.” You are:
- Sustaining cerebral perfusion
- Preserving myocardium
- Protecting kidneys
- Controlling inflammation
- Balancing coagulation
CPB Technology and Techniques directly decide patient survival. Mastery is not optional—it’s your professional duty.
Frequently Asked Questions (FAQ)
What is the main goal of CPB?
To temporarily replace heart and lung function while maintaining systemic perfusion and oxygenation.
Why are centrifugal pumps preferred today?
They reduce hemolysis, are pressure-dependent, and offer higher safety.
What ACT is required for CPB?
Typically > 400–480 seconds, depending on institutional protocol.
What is the role of ultrafiltration in CPB?
It concentrates blood, reduces inflammatory mediators, and improves post-bypass recovery.
Is CPB safer today than before?
Yes. With modern coatings, monitoring, and automation, CPB safety has dramatically improved.
People Also Ask
What are the latest developments in CPB technology?
Mini-circuits, AI-integrated monitoring, smart oxygenators, and automatic safety controls.
How does CPB affect the brain?
Through microembolism, hypoperfusion, and inflammation—prevented via filters and NIRS monitoring.
What is the difference between CPB and ECMO?
CPB is short-term intraoperative support; ECMO is long-term ICU support.
Can CPB cause kidney injury?
Yes, but optimized flow, MAP control, and ultrafiltration reduce the risk.
What skills must a perfusionist master for safe CPB?
Hemodynamics, gas exchange, anticoagulation, ultrafiltration, monitoring, and crisis management.

Final Takeaway – The Perfusionist Is the Brain Behind the Bypass
CPB Technology and Techniques are evolving fast—but the perfusionist remains the critical control center. Machines support the circulation, but your clinical judgment supports life.
From oxygenation to anticoagulation, from temperature to microcirculation—every parameter you control shapes the patient’s outcome. As cardiac surgery advances, perfusionists are no longer backstage professionals—we are front-line clinical strategists.
If you master CPB Technology and Techniques, you don’t just assist surgery—you define its success. Stay sharp. Stay data-driven. And keep leading from the pump.
What is CPB technology used for?
CPB technology is used to support circulation, oxygenation, temperature control, and metabolic stability during open-heart surgery.
Who operates the CPB machine?
A certified clinical perfusionist operates and manages all CPB technology.
Is CPB considered life support?
Yes. CPB is a full temporary life-support system for the heart and lungs.