Table of Contents
- What Is Cardiopulmonary Bypass (CPB) and How It Impacts Surgery?
- The Long-Term Cardiovascular Effects of CPB technology
- Kidney Complications During and After Cardiopulmonary Bypass (CPB)
- The Inflammatory Response Triggered by heart-lung machine
- How Cardiopulmonary Bypass (CPB) Contributes to Postoperative Cognitive Disorders
- Key Risk Factors for CPB technology Complications
- Managing Cardiopulmonary Bypass (CPB) in High-Risk Heart Patients
- Innovations in heart-lung machine Technology for Better Patient Outcomes
- Is Cardiopulmonary Bypass (CPB) More Effective Than Off-Pump Coronary Artery Bypass?
- The Ethics of Cardiopulmonary Bypass (CPB): What Surgeons Need to Know
- Effective Strategies to Minimize Cardiopulmonary Bypass (CPB) Risks
- Cardiopulmonary Bypass (CPB) in Heart Transplant Surgery: A Vital Role
- Blood Coagulation Challenges During Cardiopulmonary Bypass (CPB)
- Exploring the Various Cardiopulmonary Bypass (CPB) Circuit Types
- The pathophysiology of cardiopulmonary bypass in pediatric patients.
- Future Directions in CPB Research
- Frequently Asked Questions (FAQs)
1.What Is Cardiopulmonary Bypass (CPB) and How It Impacts Surgery?
In cardiac surgery, cardiopulmonary bypass (CPB) is often necessary, but it comes with significant pathophysiological effects. These effects, including systemic inflammation and organ dysfunction, are inherent to the procedure and influence patient outcomes. The pathophysiology of CPB can alter heart and kidney function, leading to long-term complications such as myocardial injury and renal failure.
2.The Long-Term Cardiovascular Effects of CPB technology
CPB alters myocardial physiology through ischemia-reperfusion injury, oxidative stress, and inflammation. Over time, patients may develop:
- Myocardial dysfunction due to microvascular damage.
- Fibrotic remodeling, leading to diastolic dysfunction.
- Arrhythmias, particularly atrial fibrillation, postoperatively.
- Reduced left ventricular function, causing heart failure symptoms.
- Coronary microvascular dysfunction, impairing oxygen delivery.
- Increased myocardial oxygen demand, leading to ischemic events.
- Endothelial dysfunction, contributing to long-term vascular disease.
3.Kidney Complications During and After Cardiopulmonary Bypass (CPB)
Renal impairment is a well-documented complication of Cardiac bypass due to reduced renal perfusion and inflammatory damage. Risk factors include:
- Prolonged CPB time, leading to acute kidney injury (AKI).
- Hemolysis-induced hemoglobinuria, which can cause tubular obstruction.
- Inflammatory cytokine release, exacerbating renal stress.
- Microemboli-induced renal ischemia, impairing function.
- High levels of oxidative stress, leading to nephron injury.
- Use of vasopressors, which may compromise renal perfusion.
- Pre-existing renal disease, increasing susceptibility to injury.
4.The Inflammatory Response Triggered by heart-lung machine
heart-lung machine triggers a systemic inflammatory response syndrome (SIRS) due to:
- Contact between blood and artificial surfaces, activating leukocytes.
- Release of pro-inflammatory cytokines (IL-6, TNF-α, IL-1β).
- Activation of complement and coagulation pathways, worsening inflammation.
- Increased oxidative stress, leading to endothelial damage.
- Leukocyte sequestration, causing microvascular obstruction.
- Alterations in vascular permeability, contributing to fluid imbalance.
- Systemic immune dysregulation, predisposing to infections.

5.How Cardiopulmonary Bypass (CPB) Contributes to Postoperative Cognitive Disorders
Postoperative cognitive dysfunction (POCD) and delirium are concerns after CPB, attributed to:
- Microemboli from air bubbles or aortic manipulation.
- Inflammatory mediators affecting the blood-brain barrier.
- Hypoperfusion, leading to ischemic neuronal damage.
- Blood-brain barrier breakdown, increasing neuroinflammation.
- Prolonged sedation, contributing to cognitive impairment.
- Aging-related susceptibility, increasing POCD risk.
- Cerebral autoregulation disruption, impairing brain oxygenation.
6.Key Risk Factors for CPB technology Complications
Major risk factors include:
- Advanced age
- Pre-existing comorbidities (diabetes, hypertension)
- Prolonged CPB duration
- High systemic inflammatory burden
- Blood product transfusions, increasing immunological response.
- Obesity, affecting circulation dynamics.
- Poor preoperative functional status, impairing recovery.
- Inadequate myocardial protection, leading to ischemic injury.
7.Managing Cardiopulmonary Bypass (CPB) in High-Risk Heart Patients
Patients with heart failure, valvular disease, or prior cardiac interventions require tailored CPB management, including:
- Optimized myocardial protection strategies
- Individualized anticoagulation regimens
- Improved perioperative monitoring
- Use of advanced hemodynamic support devices
- Targeted vasopressor and inotropic use
- Minimized CPB duration
- Selective cerebral perfusion for at-risk patients
- Multidisciplinary team involvement
8.Innovations in heart-lung machine Technology for Better Patient Outcomes
The field of heart-lung machine technology has seen considerable advancements in recent years, focused on improving patient outcomes, reducing complications, and enhancing the efficiency of the procedure. Some key developments include:
- Miniaturized CPB Systems: Newer, more compact CPB systems reduce the overall volume of blood needed for priming, decreasing hemodilution and the need for blood transfusions. This miniaturization also aids in reducing the burden of cardiovascular and renal complications post-surgery.
- Biocompatible Coatings: Research into biocompatible coatings for CPB circuits is helping to reduce the inflammatory response triggered by artificial surfaces. Coatings that minimize platelet adhesion and activation have been shown to lower the risk of thromboembolic events and improve patient outcomes.
- Artificial Intelligence (AI) in Monitoring: AI-driven technologies are improving real-time monitoring of CPB parameters. These systems can analyze vast amounts of data from sensors embedded in the CPB circuit to optimize perfusion and detect potential issues early, preventing complications.
- Enhanced Oxygenation Membranes: New oxygenators and perfusion membranes have been developed to improve gas exchange during CPB, ensuring better oxygenation and carbon dioxide removal, which reduces the likelihood of ischemic injury during surgery.
- Non-blood Priming Solutions: Recent advancements in priming solutions that do not require blood have shown potential in reducing the need for blood products, thus mitigating the risks associated with transfusions like immune responses and infections.
9.Is Cardiopulmonary Bypass (CPB) More Effective Than Off-Pump Coronary Artery Bypass?
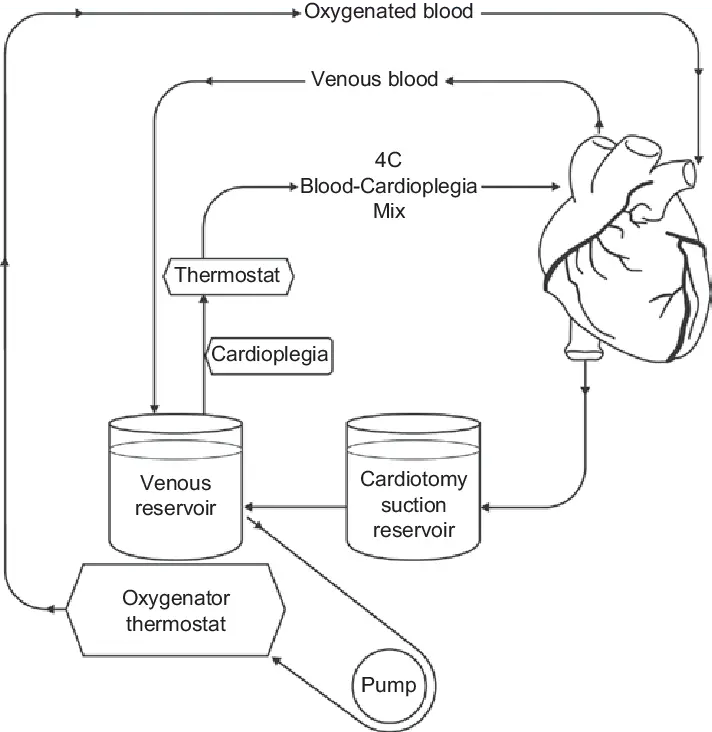
CPB and off-pump coronary artery bypass grafting (OPCAB) are both used in coronary artery bypass grafting (CABG), but they differ significantly in approach and outcomes.
- Mechanism of Action: CPB involves temporarily diverting blood flow from the heart and lungs using a heart-lung machine, while OPCAB is performed without stopping the heart, meaning the heart continues to pump while the surgeon works.
- Risks and Benefits:
- CPB: Although CPB allows for better visualization and stable conditions for grafting, it increases the risk of complications like inflammatory responses, organ dysfunction, and neurocognitive disorders post-surgery.
- OPCAB: OPCAB avoids the risks associated with CPB, such as ischemia-reperfusion injury. However, it requires more advanced surgical skill and might not be suitable for all patients, especially those with complex coronary artery disease.
- Outcomes: Studies have shown that OPCAB may reduce the incidence of neurological complications, renal dysfunction, and systemic inflammatory response compared to traditional CABG with CPB. However, OPCAB is technically more challenging and may have a higher risk of incomplete revascularization in certain patients.
10.The Ethics of Cardiopulmonary Bypass (CPB): What Surgeons Need to Know
CPB, while life-saving, raises several ethical issues that must be carefully considered:
- Patient Consent: Ensuring that patients fully understand the risks associated with CPB, including potential long-term effects on organ function and quality of life, is crucial.
- Informed Decision-Making: Surgeons must provide adequate information regarding the choice between CPB and alternative methods (e.g., OPCAB). Ensuring that patients or their families are involved in decision-making is part of ethical practice.
- End-of-Life Considerations: CPB is used in heart transplantation, which involves significant ethical challenges, such as organ allocation, informed consent for use of donor organs, and dealing with families during end-of-life decision-making processes.
- Risk of Harm: Despite its benefits, CPB can cause significant complications. Surgeons and perfusionists must weigh the potential benefits of surgery against the risks to individual patients, particularly in those with co-morbid conditions.
11.Effective Strategies to Minimize Cardiopulmonary Bypass (CPB) Risks
Reducing the risks associated with CPB is crucial for improving patient outcomes. Several strategies include:
- Optimizing Myocardial Protection: Techniques such as cold cardioplegia and warm blood cardioplegia, along with better delivery systems, protect the myocardium during the procedure, reducing ischemic damage.
- Minimizing CPB Duration: Shortening the duration of CPB reduces exposure to the inflammatory effects and improves recovery time. Surgeons should aim for efficient procedures and early decision-making to avoid prolonged bypass times.
- Use of Biocompatible Materials: Incorporating biocompatible circuits and oxygenators helps reduce the inflammatory response, improving outcomes and decreasing the likelihood of post-operative complications.
- Hemodynamic Management: Maintaining optimal perfusion pressures, temperatures, and electrolyte levels during CPB helps ensure that tissues receive adequate oxygenation and reduces the risk of organ damage.
- Anticoagulation Management: Careful management of anticoagulation during CPB is critical to prevent clotting and minimize bleeding risks. Using strategies like heparin titration based on activated clotting time (ACT) monitoring can help balance risks.
12.Cardiopulmonary Bypass (CPB) in Heart Transplant Surgery: A Vital Role
In heart transplantation, CPB plays a vital role:
- Preserving the Donor Heart: CPB helps maintain circulation in the donor heart while it is removed from the donor body and preserved for transplantation.
- Maintaining Systemic Circulation: During the transplant procedure, CPB is used to maintain systemic circulation, oxygenation, and perfusion of the organs while the recipient’s heart is removed.
- Improved Graft Survival: Advanced techniques in CPB during transplantation, including better myocardial protection and real-time monitoring, have improved heart graft survival and post-operative recovery.
13.Blood Coagulation Challenges During Cardiopulmonary Bypass (CPB)
CPB can significantly affect blood coagulation and clot formation:
- Platelet Activation: The contact of blood with artificial surfaces during CPB activates platelets, which can lead to clot formation or excessive bleeding.
- Coagulation Cascade Activation: The mechanical disruption of blood cells and the release of pro-inflammatory cytokines during CPB activate the coagulation cascade, which can result in both thromboembolic events and bleeding complications.
- Heparin and Anticoagulation Therapy: Anticoagulants like heparin are used to manage coagulation during CPB, but their use must be carefully monitored to avoid excessive bleeding or thrombosis.
- Hemodilution: The use of large volumes of priming solution for CPB can dilute the blood, affecting the balance of clotting factors and increasing the risk of bleeding.
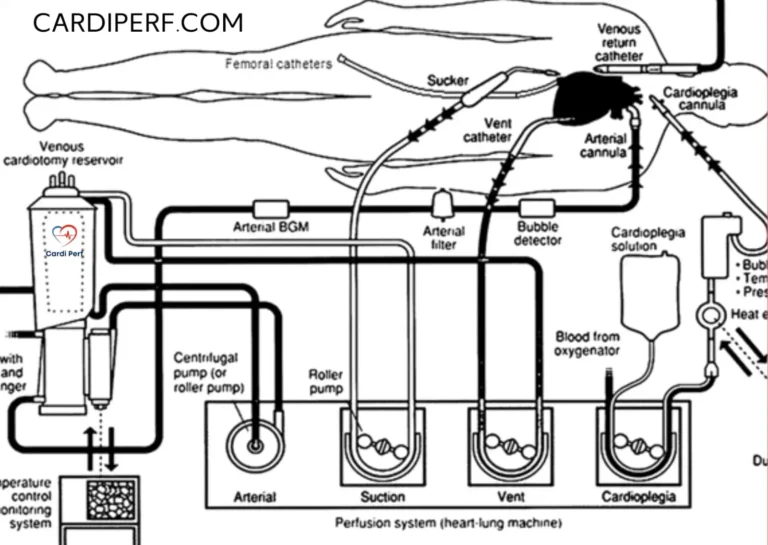
14.Exploring the Various Cardiopulmonary Bypass (CPB) Circuit Types
There are different types of CPB circuits, each designed for specific patient needs:
- Roller Pump Circuits: These circuits use a mechanical roller to move blood through the circuit. They are commonly used but can lead to hemolysis due to the shear forces generated.
- Centrifugal Pump Circuits: These pumps use a rotating impeller to move blood, offering a more gentle flow that reduces hemolysis and is considered less damaging to blood cells.
- Venous Reservoirs: The venous reservoir collects blood returned from the patient, ensuring a continuous flow into the pump. Newer designs aim to minimize blood stasis and reduce clot formation.
- Oxygenators: Modern oxygenators are designed to provide efficient gas exchange while minimizing the inflammatory response. Membrane oxygenators are commonly used, but new developments focus on improving oxygen transfer while reducing the use of blood products.
15.The Pathophysiology of Cardiopulmonary Bypass in Pediatric Patients
In pediatric patients, CPB presents unique challenges due to their smaller body size and different physiological needs:
- Smaller Circulatory System: Pediatric patients require specially designed CPB circuits with smaller blood volumes and more precise flow rates to prevent over- or under-perfusion.
- Altered Myocardial Protection: Pediatric hearts are more susceptible to ischemic injury, requiring tailored myocardial protection strategies during CPB, including the use of cold blood cardioplegia and precise temperature management.
- Increased Sensitivity to Inflammation: Children, especially neonates and infants, have an immature immune system, making them more susceptible to inflammatory responses triggered by CPB.
- Perfusion Monitoring: Advanced monitoring techniques, such as near-infrared spectroscopy (NIRS), are often used to monitor cerebral oxygenation in pediatric patients to avoid neurological damage during CPB.
16.Future Directions in CPB Research
Emerging trends in CPB research focus on:
- Artificial Intelligence (AI) in CPB Monitoring: AI-driven systems analyze real-time perfusion parameters, detecting anomalies and optimizing perfusion dynamics to enhance patient safety.
- Personalized Perfusion Strategies: Advanced computational modeling and real-time biomarkers allow perfusionists to tailor perfusion variables (flow rates, hematocrit, temperature) to individual patient needs, improving outcomes and reducing complications.
- Regenerative Medicine Approaches: Research focuses on using stem cell therapies, organ-protective drugs, and bioprinting technologies to mitigate CPB-induced tissue damage, reducing inflammation and enhancing post-operative recovery.
- Development of Biocompatible CPB Circuits: To reduce inflammatory response and coagulation disturbances.
- Miniaturized CPB Systems: Improving portability and reducing prime volume.
- Oxygenation Enhancements: Advanced oxygenator membranes to improve gas exchange efficiency.
- Non-Blood Priming Solutions: Reducing hemodilution and transfusion needs.
- Preconditioning Strategies: Techniques to enhance organ tolerance to CPB stress.
9.Frequently Asked Questions (FAQs)
- What is the purpose of cardiopulmonary bypass?
- Cardiac bypass temporarily takes over heart and lung functions to allow for complex cardiac surgeries.
- How long can a patient stay on CPB?
- CPB duration varies but is typically 1-4 hours. Prolonged use increases risks.
- Does CPB cause permanent organ damage?
- In some cases, CPB can lead to long-term organ dysfunction, especially in kidneys and brain.
- How does CPB affect blood coagulation?
- CPB triggers platelet activation and consumption, increasing bleeding risks.
- Can CPB cause memory loss?
- Some patients experience cognitive decline (POCD), but effects are usually temporary.
- Are there alternatives to CPB?
- Off-pump CABG is an alternative for select cases.
- How is CPB managed in children?
- Pediatric CPB requires tailored perfusion strategies due to unique physiological needs.
- What are the latest innovations in CPB?
- Miniaturized circuits, biocompatible coatings, and AI integration are recent advancements.
- Does CPB increase infection risks?
- Yes, due to prolonged exposure to artificial surfaces and systemic inflammation.
- What future developments can improve CPB outcomes?
- AI-driven monitoring, regenerative medicine, and personalized perfusion strategies hold promise.
17.Conclusion:
understanding the pathophysiology of cardiopulmonary bypass is crucial for improving patient outcomes in cardiac surgery. Cardiopulmonary bypass (CPB) is an indispensable tool in modern cardiac surgery, enabling complex procedures by temporarily taking over the functions of the heart and lungs. However, the pathophysiological effects of CPB on the body are profound, impacting multiple organs including the heart, kidneys, and brain. The systemic inflammatory response, organ dysfunction, and coagulation disturbances are well-documented challenges that continue to shape the evolution of cardiac surgery.
Innovations in CPB technology, such as miniaturized circuits, biocompatible coatings, and the integration of AI-driven monitoring, hold promise for mitigating these risks. Additionally, personalized perfusion strategies and regenerative medicine approaches are opening new avenues for improving patient outcomes. As research progresses, the goal is to reduce the harmful effects of CPB while maximizing its life-saving potential.
Ultimately, managing the pathophysiological consequences of Cardiac bypass requires a multidisciplinary approach, with tailored strategies to address the unique needs of each patient. Understanding these impacts, along with the latest advancements in CPB, ensures that cardiac surgeons and perfusionists can continue to improve patient care and surgical outcomes, enhancing the safety and effectiveness of this life-saving technology. For relevant content visit us at cardiperf.com