Near-Infrared Spectroscopy (NIRS) is a non-invasive technology used to monitor cerebral oxygenation in real-time during cardiac surgeries, ECMO, and other critical care settings. By providing continuous data on brain oxygen levels, Cerebral oxygenation monitoring helps perfusionists, anesthesiologists, and intensivists optimize perfusion strategies, reducing the risk of neurological complications. This technique is particularly valuable for cerebral perfusion monitoring and preventing hypoxia-related damage.
Table of Contents
- What is Near-Infrared Spectroscopy (NIRS)?
- How NIRS Works
- NIRS Pads and Application
- Analyzing NIRS Readings
- Normal and Critical NIRS Values
- Popular NIRS Devices & Manufacturers
- Clinical Applications of NIRS
- Frequently Asked Questions (FAQs)
- Conclusion
NIRS in Cardiac Surgery: What Perfusionists Need to Know?
Near-Infrared Spectroscopy (NIRS) is particularly valuable for cerebral oxygenation monitoring, cerebral perfusion tracking, and preventing hypoxia-related damage. It works by using near-infrared light to penetrate brain tissue and detect changes in oxygenated and deoxygenated hemoglobin levels. This technology is increasingly used in cardiac surgery, ECMO, and neonatal care to ensure optimal brain oxygenation levels.
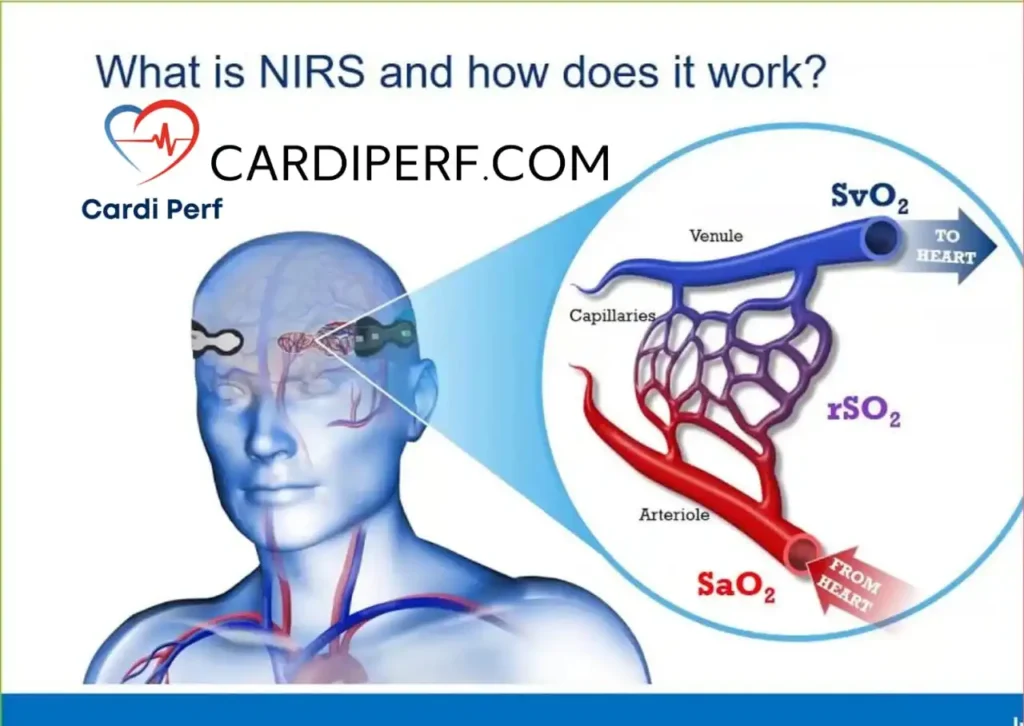
How Near-Infrared Spectroscopy (NIRS) Works to Monitor Cerebral Oxygenation
- Emission of Near-Infrared Light: Light penetrates the skull and interacts with brain tissue.
- Absorption and Reflection Analysis: The amount of light absorbed by oxygenated vs. deoxygenated hemoglobin is measured.
- Real-Time Monitoring: These readings provide insight into cerebral perfusion and oxygenation status, helping to prevent ischemic injury.
NIRS Pads and Application
How to Apply NIRS Pads Correctly
Proper pad placement is crucial for accurate readings. Follow these steps:
- Skin Preparation: Clean and dry the forehead to remove oils and debris.
- Pad Positioning: Place NIRS pads bilaterally on the forehead, ensuring correct alignment above the frontal lobes.
- Firm Attachment: Secure pads firmly but avoid excessive pressure to prevent skin irritation.
- Check Signal Quality: Ensure the device detects consistent and stable readings before proceeding with monitoring.
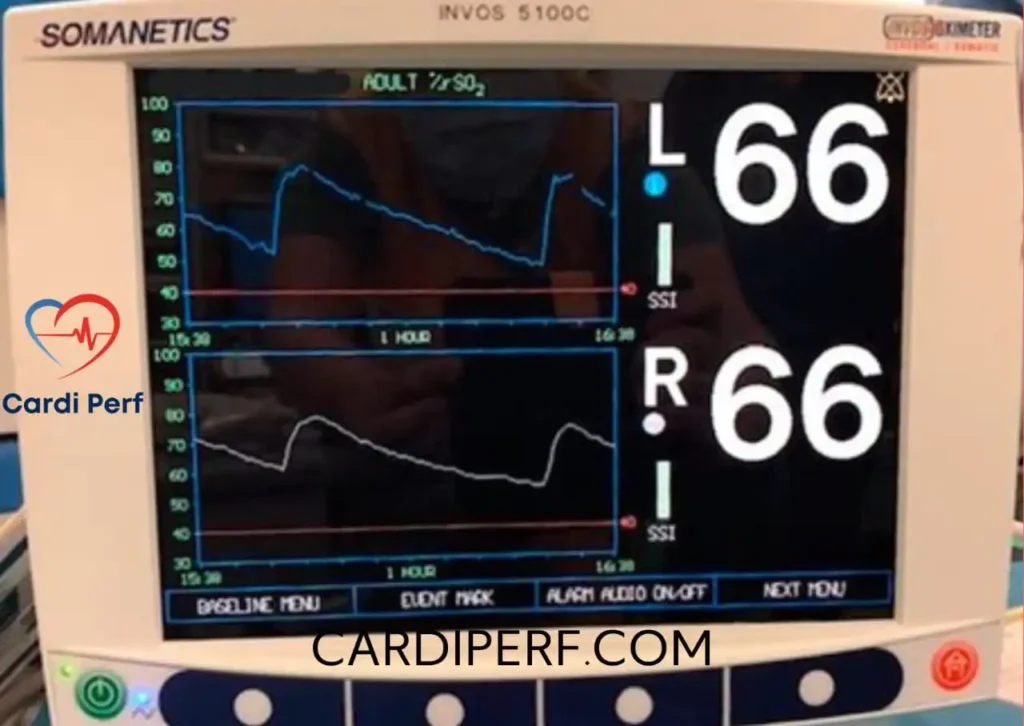
Analyzing NIRS Readings
What Should the Brain oxygen saturation Values Be?
- Normal rSO₂ Range: 60–80%
- Mild Hypoxia: 50–59%
- Critical Hypoxia: Below 50%
If values drop below 50%, urgent interventions like increasing oxygen delivery or modifying perfusion strategies are necessary.
Interpreting NIRS Fluctuations
- Sudden Decrease: Indicates cerebral ischemia or hypoperfusion.
- Gradual Decline: May suggest metabolic imbalance or inadequate ventilation.
- Asymmetrical Readings: Could indicate vascular occlusion or improper sensor placement.
NIRS rSO₂ Ranges: Normal Values, Danger Zones & Intervention Thresholds
Monitoring regional cerebral oxygen saturation (rSO₂) using Near-Infrared Spectroscopy (NIRS) is one of the fastest ways to detect cerebral hypoperfusion during cardiac surgery, ECMO, and high-risk anesthesia cases. Understanding what’s normal, what’s dangerous, and when you need to jump in with corrections is essential for preventing neurological injury.
Normal rSO₂ Values (Adults vs Pediatrics)
Keyword focus: normal NIRS values, cerebral oxygenation ranges, rSO₂ perfusion monitoring
Under stable conditions, rSO₂ values reflect the balance between cerebral oxygen supply and metabolic demand. Because pediatric patients have higher cerebral blood flow and metabolic rates, their normal values differ significantly from adults.
| Patient Group | Normal rSO₂ Range | Clinical Insight |
|---|---|---|
| Adults | 55–75% (Target ≥60%) | Reflects stable cerebral perfusion and oxygen delivery. |
| Pediatrics (Neonates/Infants/Children) | 60–80% | Higher baseline cerebral flow → higher rSO₂ readings. |
Pro Tip: Always document the baseline rSO₂ pre-induction; trends matter more than numbers.
Danger rSO₂ Values You Should Not Ignore
Keyword focus: NIRS danger values, low rSO₂, cerebral desaturation
Even short episodes of cerebral desaturation can lead to postoperative cognitive dysfunction or stroke. These thresholds indicate significant cerebral hypoxia:
| Category | Adults | Pediatrics | Meaning |
|---|---|---|---|
| Absolute Danger Value | <50% | <55% | Immediate threat to cerebral oxygenation. |
| Relative Drop (from baseline) | ≥20% | ≥20% | More predictive of injury than raw values. |
| Critical Threshold (Sustained) | <40% for 30–60 sec | <45% for 20–30 sec | High risk of ischemic injury → act fast. |
Rule of Thumb: If rSO₂ drops >20%, don’t wait — assume cerebral ischemia until proven otherwise.
When to Intervene: Perfusion Team Action Plan
Keyword focus: rSO₂ intervention, how to fix low NIRS, cardiac surgery cerebral oxygenation
When rSO₂ starts falling, your goal is to rapidly restore cerebral oxygen delivery. Prioritize corrections in this order:
1. Oxygenation
- Increase FiO₂.
- Ensure proper ventilation → check CO₂ levels (PaCO₂ impacts cerebral blood flow).
2. Pump Flow
- Increase flow rate if on CPB or ECMO.
- Assess venous drainage — poor drainage = low cerebral perfusion.
3. Hemoglobin
- Check Hct and Hb on pump.
- Transfuse if needed, especially if Hct <20% (adults) or <25% (peds).
4. Blood Pressure (MAP)
- Optimize MAP → target 60–70 mmHg adults, higher for peds.
- Adjust anesthetic depth if hypotension is drug-related.
5. Mechanical / Technical Checks
- Confirm cannula position (aortic, venous, or ECMO cannula).
- Rule out carotid compression from head position or drapes.
High-Yield Perfusion Insights
Keyword focus: cerebral desaturation management, NIRS trends, perfusion best practices
- Trends beat numbers — a stable rSO₂ baseline is gold.
- If cerebral + somatic NIRS both drop → think systemic issue (flow, FiO₂, Hb).
- If only cerebral drops → think regional issue (cannula malposition, carotid perfusion).
- Pediatric brains are more sensitive → intervene faster and more aggressively.
- rSO₂ correlates strongly with neuro outcomes — preventing drops is easier than fixing them.
✔️ Troubleshooting Cheat-Sheet
| Drop in NIRS | Likely Cause | Perfusionist Action |
|---|---|---|
| Sudden ↓ | Cannula malposition / hypotension | ↑ Flow, recheck cannula, optimize MAP |
| Gradual ↓ | Hypoventilation, ↓ FiO₂ | Adjust sweep, ↑ FiO₂ |
| Unilateral ↓ | Pad issue / carotid issue | Re-apply pad, evaluate perfusion |
Popular NIRS Devices & Manufacturers
Several industry leaders provide cutting-edge NIRS technology:
- Medtronic INVOS™ System – Highly reliable with wide clinical adoption.
- Masimo O3® Regional Oximetry – Features advanced signal processing.
- Nonin SenSmart™ Model X-100 – Known for multi-parameter monitoring.
- Edwards ForeSight™ Elite – Provides accurate tissue oxygenation trends.
Each device varies in features, sensitivity, and compatibility with hospital systems.
Clinical Applications of Cerebral oxygenation monitoring
Cerebral oxygenation monitoring is widely used in:
- Cardiac Surgery: Prevents neurological deficits during cardiopulmonary bypass (CPB).
- ECMO Patients: Ensures adequate oxygenation in critical care settings.
- Neonatal Care: Monitors oxygen levels in premature infants.
- Neurosurgery & Stroke Management: Detects cerebral hypoxia in real-time.
NIRS rSO₂ Ranges: Normal Values, Danger Zones & Intervention Thresholds
Monitoring regional cerebral oxygen saturation (rSO₂) using Near-Infrared Spectroscopy (NIRS) is one of the fastest ways to detect cerebral hypoperfusion during cardiac surgery, ECMO, and high-risk anesthesia cases. Understanding what’s normal, what’s dangerous, and when you need to jump in with corrections is essential for preventing neurological injury.
Normal rSO₂ Values (Adults vs Pediatrics)
Keyword focus: normal NIRS values, cerebral oxygenation ranges, rSO₂ perfusion monitoring
Under stable conditions, rSO₂ values reflect the balance between cerebral oxygen supply and metabolic demand. Because pediatric patients have higher cerebral blood flow and metabolic rates, their normal values differ significantly from adults.
| Patient Group | Normal rSO₂ Range | Clinical Insight |
|---|---|---|
| Adults | 55–75% (Target ≥60%) | Reflects stable cerebral perfusion and oxygen delivery. |
| Pediatrics (Neonates/Infants/Children) | 60–80% | Higher baseline cerebral flow → higher rSO₂ readings. |
Pro Tip: Always document the baseline rSO₂ pre-induction; trends matter more than numbers.
Danger rSO₂ Values You Should Not Ignore
Keyword focus: NIRS danger values, low rSO₂, cerebral desaturation
Even short episodes of cerebral desaturation can lead to postoperative cognitive dysfunction or stroke. These thresholds indicate significant cerebral hypoxia:
| Category | Adults | Pediatrics | Meaning |
|---|---|---|---|
| Absolute Danger Value | <50% | <55% | Immediate threat to cerebral oxygenation. |
| Relative Drop (from baseline) | ≥20% | ≥20% | More predictive of injury than raw values. |
| Critical Threshold (Sustained) | <40% for 30–60 sec | <45% for 20–30 sec | High risk of ischemic injury → act fast. |
Rule of Thumb: If rSO₂ drops >20%, don’t wait — assume cerebral ischemia until proven otherwise.
When to Intervene: Perfusion Team Action Plan
Keyword focus: rSO₂ intervention, how to fix low NIRS, cardiac surgery cerebral oxygenation
When rSO₂ starts falling, your goal is to rapidly restore cerebral oxygen delivery. Prioritize corrections in this order:
1. Oxygenation
- Increase FiO₂.
- Ensure proper ventilation → check CO₂ levels (PaCO₂ impacts cerebral blood flow).
2. Pump Flow
- Increase flow rate if on CPB or ECMO.
- Assess venous drainage — poor drainage = low cerebral perfusion.
3. Hemoglobin
- Check Hct and Hb on pump.
- Transfuse if needed, especially if Hct <20% (adults) or <25% (peds).
4. Blood Pressure (MAP)
- Optimize MAP → target 60–70 mmHg adults, higher for peds.
- Adjust anesthetic depth if hypotension is drug-related.
5. Mechanical / Technical Checks
- Confirm cannula position (aortic, venous, or ECMO cannula).
- Rule out carotid compression from head position or drapes.
High-Yield Perfusion Insights
Keyword focus: cerebral desaturation management, NIRS trends, perfusion best practices
- Trends beat numbers — a stable rSO₂ baseline is gold.
- If cerebral + somatic NIRS both drop → think systemic issue (flow, FiO₂, Hb).
- If only cerebral drops → think regional issue (cannula malposition, carotid perfusion).
- Pediatric brains are more sensitive → intervene faster and more aggressively.
- rSO₂ correlates strongly with neuro outcomes — preventing drops is easier than fixing them.
Near-Infrared Spectroscopy Device, Principle, and Cost
A typical NIRS device consists of a light source, optical sensors, and a monitor that displays real-time oxygenation trends. The principle behind NIRS is based on the differential absorption of near-infrared light by oxygenated versus deoxygenated hemoglobin, allowing continuous estimation of tissue oxygen saturation. These devices are compact and can be used in operating rooms, ICUs, and neonatal care units. While the price of a NIRS system varies depending on brand and features, investing in this technology is increasingly common in advanced cardiac and pediatric care due to its ability to improve patient safety and outcomes.
Frequently Asked Questions (FAQs)
1. What is the primary purpose of NIRS in cardiac surgery?
NIRS monitors cerebral oxygenation, helping to prevent neurological complications during cardiopulmonary bypass (CPB).
2. How often should NIRS readings be checked?
NIRS provides real-time monitoring, so readings should be checked continuously throughout surgery or critical care management.
3. What factors can affect NIRS readings?
Factors like hypotension, hypoxia, CO₂ levels, improper pad placement, and device calibration can impact readings.
4. Can NIRS be used in pediatric patients?
Near-Infrared Spectroscopy (NIRS) is particularly valuable for cerebral oxygenation monitoring, cerebral perfusion tracking, and preventing hypoxia-related damage.
5. What interventions can be done if NIRS values drop?
Actions may include increasing oxygen delivery, adjusting perfusion parameters, optimizing MAP, or repositioning NIRS sensors.
6. What is the difference between NIRS and pulse oximetry?
Pulse oximetry measures systemic arterial oxygen saturation, Regional oxygen saturation (rSO₂) whereas NIRS provides regional brain oxygenation data.
7. Can NIRS detect ischemic strokes?
Yes, NIRS can detect regional oxygen desaturation, which may indicate a developing stroke or hypoxic event.
8. Is NIRS technology expensive?
While initial costs can be high, NIRS technology improves patient safety, potentially reducing postoperative complications.
9. Do all hospitals use NIRS monitoring?
NIRS usage varies depending on hospital protocols, surgical complexity, and resource availability.
10. Are there any risks associated with NIRS?
NIRS is a non-invasive technology with no known risks, though improper sensor application may lead to inaccurate readings.
Conclusion
Near-Infrared Spectroscopy (NIRS) has become an essential tool in perfusion and critical care, offering real-time insights into cerebral oxygenation. Proper application of NIRS pads and accurate interpretation of readings ensure optimal patient outcomes.
With advancements in AI-driven analysis and device integration, NIRS is set to revolutionize cerebral monitoring in the future. visit us at cardiperf.com
🔗 Related Articles:
- Goal-Directed Perfusion and NIRS
- Advanced Monitoring in Perfusion
- Optimizing Cerebral Oxygenation in Surgery
📢 Have you used NIRS in clinical practice? Share your insights in the comments!