CPB Filtration Best Practices are essential for minimizing risks and optimizing patient outcomes during cardiopulmonary bypass (CPB). CPB, a cornerstone of modern cardiac surgery, enables surgeons to operate on a still, bloodless heart. However, diverting blood through an extracorporeal circuit introduces potential risks, including embolization, inflammation, and organ dysfunction. Effective filtration, as outlined in these best practices, is paramount to mitigating these risks and ensuring patient safety. This comprehensive guide delves into the intricacies of CPB filtration, exploring the various types of filters, their functions, and their critical role in optimizing patient outcomes.
I. Introduction: The Unsung Heroes of CPB
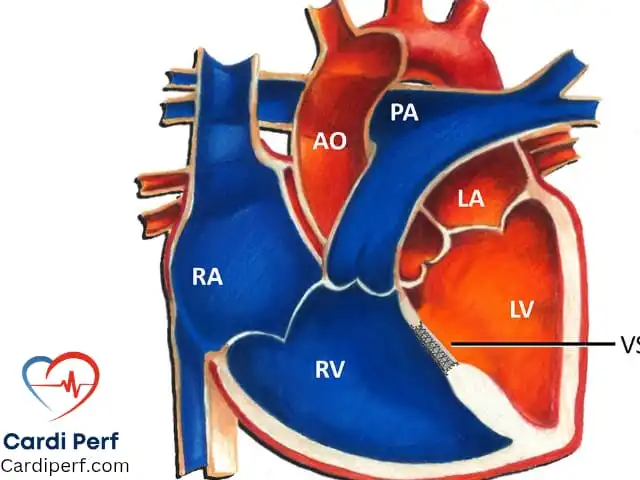
CPB involves temporarily taking over the function of the heart and lungs, circulating and oxygenating blood outside the body. While this technology has revolutionized cardiac surgery, it also presents unique challenges. The exposure of blood to artificial surfaces, the generation of microemboli, and the activation of inflammatory pathways can lead to significant complications. This is where filtration steps in, acting as a crucial safeguard to protect the patient.
Proper filtration during CPB is not merely a technical detail; it is a fundamental aspect of patient care. By removing harmful particles, air bubbles, and inflammatory mediators, filters contribute significantly to minimizing postoperative morbidity and mortality. This article will provide an in-depth look at the different types of filters used in CPB, their specific roles, and the science behind their design.
II.Pre-Bypass Filtration: The First Step in CPB Filtration Best Practices
A. Preparing for a Clean Circuit
Before initiating CPB, the priming solution used to fill the circuit must be meticulously filtered. The pre-bypass filter plays a vital role in removing any particulate matter, manufacturing debris, or potential contaminants that may have entered the solution during preparation.
B. Pore Size and Importance
Typically, pre-bypass filters have a pore size of 0.2–5 µm. This fine filtration is crucial for preventing the introduction of even the smallest particles into the patient’s circulation. By removing these potential emboli, the risk of early complications and inflammatory reactions is significantly reduced. Once CPB is initiated, this filter is removed from the circuit, as the primary filtration duties are then handled by the arterial line filter.
C. Preventing Early Embolization
The importance of pre-bypass filtration cannot be overstated. By ensuring a clean priming solution, perfusionists set the stage for a safe and successful CPB run. This meticulous step is essential for blood purification in CPB and embolic protection in surgery.
III. Arterial Line Filtration: A Key Component of CPB Filtration Best Practices
A. The Role of the Arterial Line Filter

The arterial line filter is the primary filter responsible for removing particulate matter from the blood before it is returned to the patient. It is designed to capture microemboli removal, air bubble filtration, and other debris that may have accumulated during the CPB run.
B. Placement and Function
This filter is strategically placed in the arterial line, just before the blood enters the arterial cannula and returns to the patient’s systemic circulation. Its location ensures that the blood is thoroughly filtered immediately before re-entering the body.
C. Pore Size and Clinical Significance
Arterial line filters typically have a pore size of 20–40 µm. This pore size is optimized to remove clinically significant particles while maintaining adequate blood flow. The effectiveness of this filtration is crucial for arterial filter placement and CPB circuit safety.
IV. Gas Filtration: Ensuring Optimal Oxygenation
A. The Importance of Gas Filters
Gas filters in CPB, also known as oxygenator filters, play a critical role in removing gaseous microemboli from the blood. These filters are essential for maintaining the efficiency of gas exchange within the oxygenator and preventing gaseous embolism prevention in accordance with CPB Filtration Best Practices
B. Placement and Function within the Oxygenator
These filters are either integrated within the oxygenator or placed as separate filters in the gas supply line. Their function is to remove microbubbles and other gaseous emboli that may form during the oxygenation process.
C. Pore Size and Significance
Gas filters typically have a pore size of 0.2–5 µm. This fine filtration ensures that even the smallest gas bubbles are removed, reducing the risk of air embolism and maintaining optimal oxygenator filter function. They utilize membrane filtration in CPB to achieve the CPB Filtration Best Practices
V. Cardiotomy Reservoir Filtration: Salvaging and Cleaning Suctioned Blood
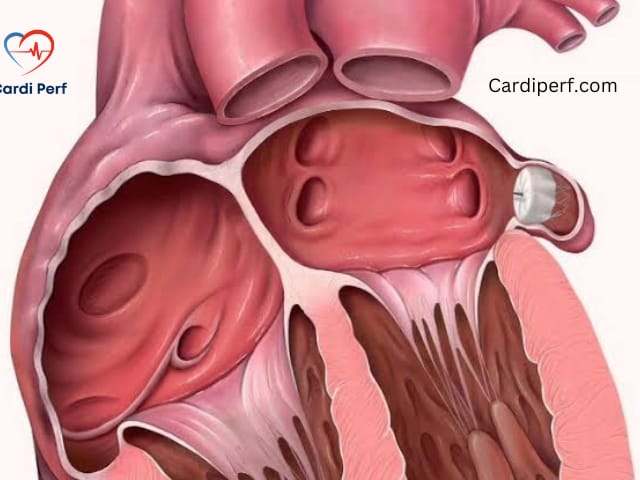
A. Role of the Cardiotomy Reservoir Filter
The cardiotomy reservoir filter is responsible for filtering suctioned blood from the surgical field before it is returned to the CPB circuit. This filter removes cellular debris, tissue fragments, and other particulate matter that may be present in the suctioned blood.
B. Placement and Function
Located within the cardiotomy reservoir, this filter ensures that the blood is cleaned before re-entering the circuit. This process is vital for suctioned blood filtration and thrombus removal in CPB.
C. Pore Size and Clinical Implications
Cardiotomy reservoir filters typically have a pore size of 20–40 µm, similar to arterial line filters. This pore size effectively removes clinically significant particles while maintaining adequate blood flow.
VI. Leukocyte-Depleting Filters: Minimizing Inflammatory Response
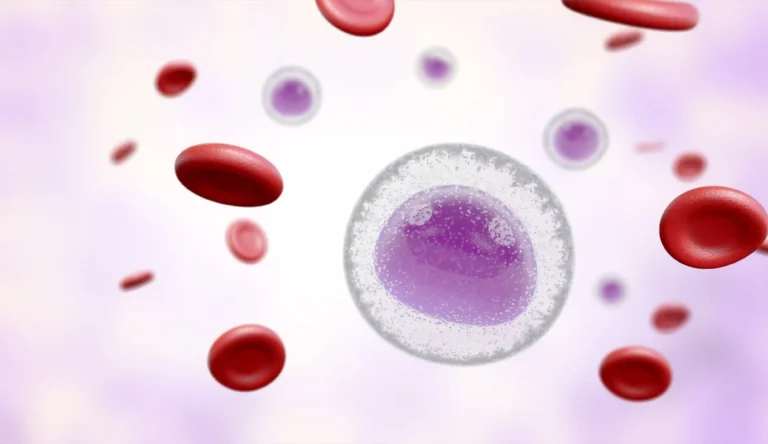
A. The Function of Leukocyte-Depleting Filters
Leukocyte-depleting filters are designed to remove white blood cells (WBCs) from the blood. This is crucial for reducing the inflammatory response in CPB and minimizing postoperative complications.
B. Applications and Benefits
These filters are commonly used in procedures such as CABG, valve surgeries, and complex cardiac procedures where inflammation control is essential. By removing WBCs, these filters help prevent microvascular dysfunction and reduce the risk of postoperative systemic inflammatory response syndrome (SIRS).
C. Placement and Use
Leukocyte-depleting filters can be placed in the arterial line or the cardioplegia circuit to remove leukocytes from transfused blood or cardioplegia solution. This process, known as leukodepletion in perfusion, is critical for improving patient outcomes in accordance with CPB Filtration Best Practices
D. Clinical Significance
The use of these filters is particularly important in patients at high risk for inflammatory complications. They are essential in CABG filter use and cardioplegia filter applications.
VII. Additional Filtration Technologies in CPB
A. Hemofilters and Hemoconcentrators
Hemofilters in CPB and hemoconcentrators in CPB are used for plasma water removal and hemoconcentration. These devices remove excess fluid from the blood, helping to maintain optimal hematocrit levels and reduce edema.
B. Bubble Trap Filters
Bubble trap filters are another type of filter used to remove air bubbles from the blood. These filters are often used in conjunction with other filtration devices to ensure thorough removal of gaseous emboli.

VIII.CPB Filtration Best Practices for Enhanced Patient Outcomes Patient Outcomes
A. Factors Affecting Filtration Efficiency
Several factors can influence the efficiency of CPB filters, including pore size, filter material, and blood flow rate. Proper filter selection and maintenance are essential for ensuring optimal filtration.
B. The Role of Perfusionists
Perfusionists play a critical role in optimizing CPB filtration. They are responsible for selecting the appropriate filters, ensuring proper placement, and monitoring filter performance throughout the CPB run.
C. Continuous Advancements
Ongoing research and technological advancements continue to improve CPB filtration. New filter materials, designs, and techniques are being developed to further enhance patient safety and minimize complications. CPB circuit optimization is a continual process.

IX. Conclusion: The Critical Role of Filtration in CPB
Effective CPB filtration is essential for minimizing complications and improving patient outcomes.
X.Frequently Asked Questions (FAQs)
1. Q: What is the primary purpose of filtration during cardiopulmonary bypass (CPB)?
A: The primary purpose of filtration during CPB is to remove harmful particles, air bubbles, and inflammatory mediators from the blood. This helps to minimize complications such as embolization, organ dysfunction, and systemic inflammatory response syndrome (SIRS), ensuring patient safety and optimal outcomes.
2. Q: Why is a pre-bypass filter necessary before initiating CPB?
A: A pre-bypass filter is essential to remove particulate matter, manufacturing debris, and potential contaminants from the priming solution. This ensures a clean circuit before blood is circulated, preventing early embolization and inflammatory reactions following CPB Filtration Best Practices
3. Q: What is the difference between an arterial line filter and a gas filter in a CPB circuit?
A: An arterial line filter removes particulate matter and air bubbles from the blood before it returns to the patient, typically with a pore size of 20-40 µm. A gas filter, integrated within the oxygenator or gas supply line, removes gaseous microemboli, usually with a pore size of 0.2-5 µm, ensuring efficient gas exchange.
4. Q: How do leukocyte-depleting filters help in reducing inflammatory responses during CPB?
A: Leukocyte-depleting filters remove white blood cells (WBCs) from the blood, which are key mediators of inflammation. By reducing the number of circulating WBCs, these filters minimize the risk of microvascular dysfunction and postoperative SIRS.
5. Q: What is the significance of pore size in CPB filters?
A: Pore size determines the size of particles that a filter can remove. Smaller pore sizes (e.g., 0.2-5 µm) remove finer particles like gaseous microemboli, while larger pore sizes (e.g., 20-40 µm) remove larger particles like cellular debris and particulate matter. Selecting the appropriate pore size is crucial for effective filtration.
6. Q: Where is the cardiotomy reservoir filter located, and what is its function?
A: The cardiotomy reservoir filter is located within the cardiotomy reservoir. Its function is to filter suctioned blood from the surgical field, removing cellular debris and tissue fragments before the blood is returned to the CPB circuit.
7. Q: Can filters prevent all complications associated with CPB?
A: While filters significantly reduce the risk of many complications, they cannot prevent all of them. Other factors, such as the patient’s underlying health conditions, surgical technique, and overall CPB management, also play crucial roles in patient outcomes.
8. Q: How often should CPB filters be changed during a procedure?
A: CPB filters are typically used for the duration of a single procedure and are not changed mid-operation unless there is a specific indication, such as a significant pressure drop or visible debris accumulation. Proper monitoring and management by the perfusionist ensure optimal filter performance.
9. Q: What advancements are being made in CPB filtration technology?
A: Advancements in CPB filtration include the development of new filter materials with improved biocompatibility and efficiency, as well as the integration of real-time monitoring systems to assess filter performance. Researchers are also exploring novel filtration techniques to further minimize inflammatory responses and improve patient outcomes.
10. Q: What is the role of the perfusionist in ensuring optimal CPB filtration?
A: The perfusionist plays a critical role in selecting the appropriate filters, ensuring proper placement, monitoring filter performance, and troubleshooting any issues that may arise during CPB. Their expertise is essential for optimizing filtration and ensuring patient safety.