Patients with a history of heparin-induced thrombocytopenia with thrombosis (HITT) pose a unique challenge when they require cardiopulmonary bypass (CPB). The anticoagulation strategy must be carefully selected to balance the risk of thrombosis and bleeding while ensuring safe CPB management. This article explores the best anticoagulation options available for such cases, the role of the anesthesia and perfusion teams, and necessary testing before, during, and after surgery.
Understanding Heparin-Induced Thrombocytopenia (HIT)
What is HIT?
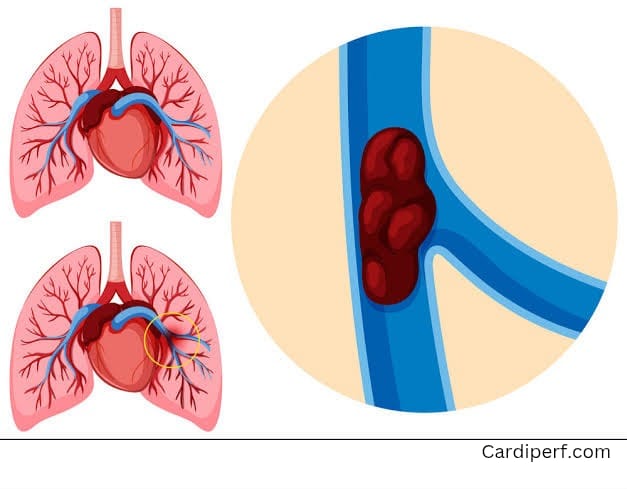
Heparin-induced thrombocytopenia (HIT) is a severe immune-mediated adverse reaction to heparin exposure, leading to significant thrombocytopenia and an increased risk of thrombosis. It occurs due to antibodies forming against platelet factor 4 (PF4)-heparin complexes, which activate platelets and provoke clot formation.
Types of HIT
- Type 1 HIT – A mild, transient drop in platelet count that typically resolves without complications.
- Type 2 HIT (HITT) – A more severe form where immune-mediated platelet activation leads to arterial and venous thrombosis.
Anticoagulation Strategy for CPB in HITT Patients
Can Heparin Be Used?
Despite a history of HITT, some patients may still be eligible for heparin use during CPB, based on the following rationale:
- Stoichiometric Effect – High-dose heparin during CPB overwhelms the formation of heparin-PF4 antibody complexes, reducing the risk of platelet activation and thrombosis.
- Antibody Clearance – Studies suggest that HIT antibodies typically clear within 50–90 days:
- 50 days for platelet activation assays.
- 85–90 days for immunoassays.
- Given a significant time gap since HITT diagnosis, circulating antibodies may not persist.
- Protamine Reversal – Complete reversal of heparin with protamine sulfate at the end of CPB further minimizes the risk of delayed immune response.
Alternative Anticoagulation Options
For patients with acute or subacute HIT, alternative strategies include:
- Bivalirudin – A direct thrombin inhibitor commonly used for CPB in HIT patients. Preferred in those with normal renal function.
- Argatroban – Another direct thrombin inhibitor, used for patients with renal impairment requiring dialysis.
- Plasma Exchange – Considered in urgent surgeries if antibodies are still present.
- Antiplatelet Therapy – Use of GPIIb/IIIa inhibitors (e.g., eptifibatide, tirofiban) can reduce platelet activation if heparin must be used.
Role of Anesthesia and Perfusionist in CPB
Anesthesia Team Responsibilities:
- Ensure optimal hemodynamic stability and monitor coagulation parameters during CPB.
- Manage anticoagulation strategy in coordination with the perfusionist and surgical team.
- Administer appropriate reversal agents post-CPB and monitor for bleeding complications.
- Ensure postoperative pain management and ventilation support.
Perfusionist Responsibilities:
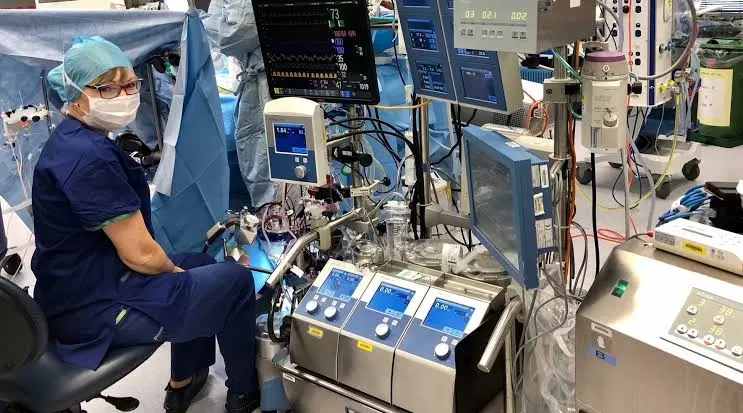
- Operate and maintain the heart-lung machine.
- Monitor blood flow, oxygenation, and anticoagulation levels throughout CPB.
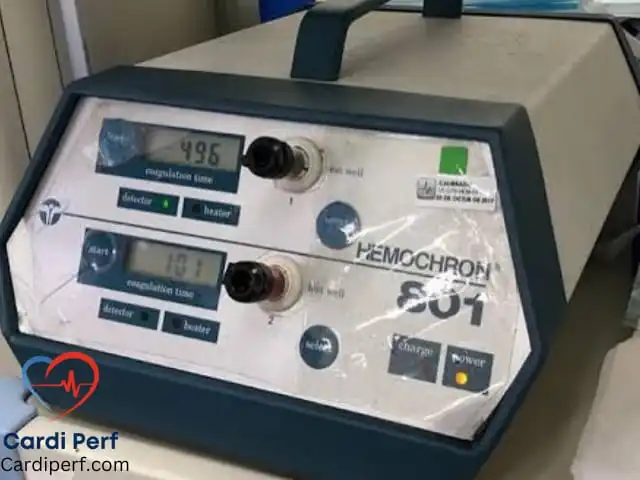
- Adjust anticoagulation dosing based on ACT (Activated Clotting Time) measurements.
- Assist in weaning the patient off CPB and manage transitions to alternative circulatory support.
Additional Tests Required Before, During, and After Bypass
Before CPB:
- HIT antibody testing (if not recently performed).
- Coagulation profile: PT, INR, aPTT, fibrinogen levels.
- Platelet count and function tests.
- DVT screening via ultrasound.
During CPB:
- ACT monitoring to ensure proper anticoagulation.
- Blood gas analysis (ABG) for oxygenation and pH balance.
- Thromboelastography (TEG) or Rotational Thromboelastometry (ROTEM) for coagulation assessment.
After CPB:
- Serial platelet counts to monitor for HIT recurrence.
- D-dimer levels to check for thrombosis.
- Echocardiography (TEE or TTE) to assess heart function post-surgery.
- Hemodynamic monitoring and follow-up coagulation studies.
Frequently Asked Questions (FAQs)
1. Can patients with HIT ever receive heparin again?
Yes, but only if they have remote HIT (negative immune and functional assays). Heparin should still be avoided in acute and subacute HIT cases.
2. What is the best alternative anticoagulant for CPB in HIT patients?
Bivalirudin is the most widely used alternative due to its direct thrombin inhibition and short half-life.
3. Why is monitoring platelet count postoperatively important?
Patients with prior HIT are at risk of delayed-onset HIT, which can occur 5–10 days after surgery, leading to life-threatening thrombosis.
4. How long should anticoagulation be continued postoperatively?
Anticoagulation should be continued until platelet count recovery to reduce the risk of thrombosis.
5. Can HIT be fatal if untreated?
Yes, HITT (HIT with thrombosis) has a high risk of severe complications, including stroke, limb ischemia, and multi-organ failure.
6. What are the symptoms of HIT?
Symptoms include rapid platelet drop, skin necrosis, deep vein thrombosis (DVT), pulmonary embolism (PE), and arterial occlusions.
7. How is HIT diagnosed?
Through clinical scoring systems (4T score), immunoassays, and functional platelet activation tests.
8. Can HIT occur after surgery even without heparin?
Yes, due to heparin exposure in flushes, heparin-coated catheters, or unrecognized previous exposure.
Key Takeaways
- Heparin can be safely used for CPB in patients with remote HIT (negative functional and immune assays).
- In acute or subacute HIT, heparin should be avoided in favor of bivalirudin, argatroban, or plasma exchange.
- Anesthesia and perfusion teams play a critical role in ensuring safe anticoagulation management and CPB performance.
- Multidisciplinary collaboration between cardiac surgery, perfusion, anesthesia, and hematology is essential for optimizing outcomes.
For more expert insights on cardiac surgery, perfusion sciences, and ECMO, visit CardiPerf.com!