The Bentall procedure is the gold standard for treating aortic root aneurysms, severe aortic regurgitation, and life-threatening aortic dissections. This complex surgical intervention involves replacing the aortic root, aortic valve, and ascending aorta while re-implanting the coronary arteries into the graft.
For cardiac surgeons, perfusionists, anesthesiologists, and critical care teams, mastering the intricacies of the Bentall procedure is crucial for optimizing patient outcomes. This article explores its indications, contraindications, surgical technique, perfusion and anesthesia strategies, femoral cannulation considerations, postoperative management, and future innovations.
Indications for the Bentall Procedure
The Bentall procedure is performed for:
- Aortic Root Aneurysms – Common in Marfan syndrome, Loeys-Dietz syndrome, and bicuspid aortic valve disease.
- Acute Type A Aortic Dissection – When the dissection involves the aortic root and valve.
- Severe Aortic Regurgitation – Resulting from annular dilation, leaflet degeneration, or endocarditis.
- Heritable Connective Tissue Disorders – High risk for aortic rupture.
- Prosthetic Valve Dysfunction – When an existing aortic prosthesis fails.
Contraindications for the Bentall Procedure
Despite being a lifesaving procedure, the Bentall operation is contraindicated in certain patients due to high surgical risks or alternative treatment options.
Absolute Contraindications
- Severe multi-organ failure – Poor prognosis despite surgical intervention.
- End-stage heart failure (non-candidate for heart transplantation or LVAD).
- Active, uncontrolled infection (e.g., infective endocarditis with sepsis).
- Severe neurological impairment (persistent coma, massive stroke, or brain death).
- Malignancy with poor prognosis (<6 months life expectancy).
Relative Contraindications
- High surgical risk (STS Score >10% mortality).
- Severe pulmonary hypertension (PA pressure >60 mmHg) with right heart failure.
- Severe frailty (low preoperative functional status, cachexia, or sarcopenia).
- Hostile chest (multiple prior sternotomies with severe adhesions, porcelain aorta, or severe calcification).
- High-risk redo operations without feasible surgical options.
In select cases, alternative options such as valve-sparing root replacement (David procedure), TEVAR (thoracic endovascular aortic repair), or hybrid approaches may be considered.
Surgical Approach
Preoperative Planning and Imaging
Before surgery, comprehensive imaging is critical:
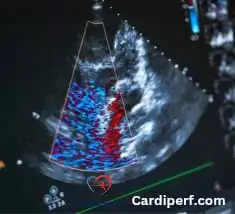
- Transthoracic or Transesophageal Echocardiography (TTE/TEE) – Evaluates valve function and ventricular performance.
- CT Angiography (CTA) – Assesses aortic dimensions, calcification, and dissection extent.
- MRI (if CTA is contraindicated) – Provides additional soft tissue details.
Cardiopulmonary Bypass (CPB) and Myocardial Protection
- Arterial Cannulation:
- Ascending aorta is preferred.
- Femoral or axillary cannulation is used in severe aortic disease or reoperative cases.
- Venous Cannulation:
- Bicaval cannulation (SVC & IVC) ensures optimal drainage.
- Myocardial Protection Strategy:
- Cold blood cardioplegia (antegrade & retrograde) is delivered every 20–30 minutes.
- Single-dose Custodiol cardioplegia is an alternative option.
- Moderate hypothermia (28–32°C) is maintained to reduce metabolic demand.
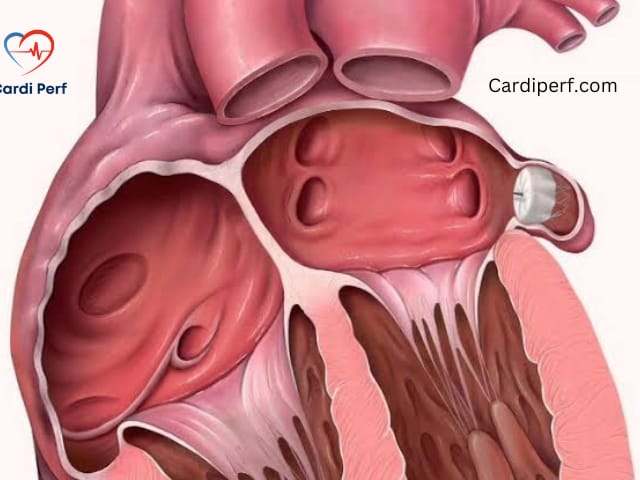
Aortic Root Excision and Coronary Reimplantation
- The diseased aortic root and valve are completely excised.
- Coronary ostia are carefully mobilized and reimplanted using the button technique to prevent tension or kinking.
Graft Selection and Valve Implantation
Surgeons must select an appropriate composite graft:
- Mechanical Valve (On-X, St. Jude, Carbomedics) – Durable but requires lifelong anticoagulation.
- Bioprosthetic Valve (Carpentier-Edwards, Medtronic Hancock II) – No anticoagulation needed but has limited durability.
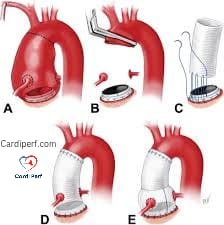
Distal Anastomosis and Weaning from CPB
- Graft is sutured to the native aorta or aortic arch.
- TEE is used post-CPB to check for leaks, valve function, and ventricular performance.
Femoral Cannulation in the Bentall Procedure
When Is Femoral Cannulation Required?
Femoral cannulation is considered in the following situations:
- Redo Sternotomy Cases – To avoid injury to patent grafts or a calcified aorta.
- Acute Type A Aortic Dissection – When the ascending aorta is compromised.
- Severe Atherosclerosis or Porcelain Aorta – Reduces embolization risk.
- Emergency Surgery with Hemodynamic Instability – Provides rapid circulatory support.
- Minimally Invasive Approach – Used in select cases.
Perfusion Considerations with Femoral Cannulation
- Challenges of Retrograde Flow:
- Risk of atherosclerotic embolization.
- Malperfusion syndrome if aortic dissection is present.
- Differential hypoxia (Harlequin syndrome).
- Strategies to Optimize Perfusion:
- TEE Monitoring to assess embolization risk.
- Higher CPB Flows (2.4–2.6 L/min/m²).
- Moderate Hypothermia (28–32°C).
- Selective Antegrade Cerebral Perfusion (ACP) if needed.
Essential Equipment for Femoral Cannulation
- Ultrasound for vascular access guidance.
- Seldinger technique kit for percutaneous insertion.
- Vascular clamps and dilators for open cannulation.
- Guidewires and fluoroscopy for precise placement.
- Distal perfusion catheter (6–8 Fr) to prevent limb ischemia.
- ACT monitoring to maintain anticoagulation (>400 seconds).
Role of Cell Saver in the Bentall Procedure:
- Minimizing Blood Loss:
- The Bentall procedure is a major surgery involving the aortic valve and the ascending aorta, and it typically requires clamping of the aorta, which can result in significant blood loss.
- The Cell Saver system helps collect and filter the patient’s own blood lost during surgery, process it to remove any contaminants (like fat, debris, and clots), and then reinfuse the filtered blood back into the patient.
- This reduces the need for allogeneic (donor) blood transfusions, which carry risks of complications such as immune reactions, infections, and transfusion-related issues.
- Improving Blood Conservation:
- Blood conservation is especially important in high-risk surgeries like the Bentall procedure. The Cell Saver helps to ensure that the patient’s own blood is used to replace lost blood, thus improving overall hemodynamic stability and reducing the need for external blood supply.
- By reinfusing processed blood, the patient’s blood volume and red blood cell count are maintained, which helps avoid anemia, hypovolemia, and potential complications related to blood loss.
- Reducing Complications:
- The use of the Cell Saver in heart surgery reduces the chance of infection or allergic reactions that could arise from donor blood transfusions.
- It can also improve recovery times as the patient’s own blood doesn’t trigger immune responses, promoting better tissue oxygenation and healing post-surgery.
- Enhancing Recovery and Reducing Hospital Stay:
- By minimizing the need for transfusions and reducing the complications associated with blood loss, the Cell Saver can contribute to a smoother recovery process and potentially shorten the length of the hospital stay post-surgery.
Cell Saver Process in the Bentall Procedure:
- Blood Collection: During the surgery, blood that is lost through surgical sites (e.g., during the aortic valve replacement and aortic root replacement) is suctioned into the Cell Saver device.
- Blood Processing: The collected blood is washed to remove contaminants and any clotted elements.
- Reinfusion: The processed blood is then reinfused back into the patient, helping to replace the blood lost during the procedure.
Advantages of Using Cell Saver in the Bentall Procedure:
- Reduces the need for allogeneic blood transfusions, minimizing associated risks.
- Helps maintain normal blood volume and oxygen-carrying capacity.
- Decreases the risk of complications like coagulopathies or excessive bleeding from transfusion.
- Improves overall surgical outcomes and patient recovery by providing a safer alternative to external blood sources
- The Cell Saver is a key tool in enhancing patient safety and blood conservation during the Bentall procedure, especially given the complexity and potential for blood loss. It supports better postoperative recovery and helps minimize reliance on donor blood.
Frequently asked questions (FAQs) about the Bentall procedure,
1. What is the Bentall procedure?
The Bentall procedure is a type of heart surgery that is performed to repair or replace the aortic valve and the aorta (the large artery that carries blood from the heart) when a patient has a condition such as an aortic aneurysm or aortic dissection. It involves replacing both the aortic valve and the ascending aorta, often using a prosthetic valve and a conduit (tube) to restore normal blood flow.
2. Why is the Bentall procedure performed?
The Bentall procedure is typically performed in cases of:
- Aortic aneurysm (dilation of the aorta)
- Aortic dissection (tear in the aorta wall)
- Congenital conditions (like Marfan syndrome)
- Severe aortic valve disease (aortic insufficiency or stenosis)
- If the aortic valve and ascending aorta need replacement simultaneously due to pathology.
3. What are the risks associated with the Bentall procedure?
As with any major surgery, the Bentall procedure carries risks such as:
- Infection
- Bleeding
- Stroke
- Heart rhythm problems (arrhythmias)
- Injury to nearby structures (e.g., the coronary arteries)
- Prosthetic valve dysfunction
- Kidney injury or failure
4. How is the Bentall procedure performed?
The procedure typically involves:
- A general anesthesia and a median sternotomy (incision through the breastbone) to access the heart.
- The aorta is clamped, and the heart is temporarily stopped using a cardioplegic solution.
- The aortic valve is replaced with a prosthetic valve.
- The diseased portion of the ascending aorta is replaced with a conduit (a synthetic tube) that contains a new valve (either mechanical or biological) for the aortic valve.
- The coronary arteries are re-implanted into the new conduit.
- Once the procedure is complete, the heart is restarted, and normal circulation is restored.
5. What type of prosthetic valve is used in the Bentall procedure?
In the Bentall procedure, the most commonly used prosthetic valves are:
- Mechanical valves: Durable, but require lifelong anticoagulation therapy.
- Biologic (tissue) valves: Less durable than mechanical valves but don’t require lifelong anticoagulation therapy.
The choice of valve depends on the patient’s age, medical condition, and preferences.
6. What is the recovery process like after the Bentall procedure?
Recovery after the Bentall procedure can be lengthy:
- Patients typically stay in the hospital for about 7-10 days, depending on their recovery.
- Full recovery can take several months (typically 3-6 months).
- During the initial recovery phase, patients may need physical therapy and regular monitoring to ensure proper healing.
- Follow-up visits to monitor heart function, valve performance, and the aorta’s condition are essential.
7. Can the Bentall procedure be performed minimally invasively?
While the traditional Bentall procedure requires a large incision (sternotomy), there are some centers that offer minimally invasive alternatives, such as:
- A mini-sternotomy (smaller incision on the chest).
- Robotic surgery (using small incisions and a robotic system for more precise movements).
However, these options depend on the specific patient’s anatomy, surgeon’s expertise, and institutional resources.
8. What are the long-term outcomes of the Bentall procedure?
Long-term outcomes after the Bentall procedure are generally positive, with most patients experiencing significant improvements in symptoms and quality of life. The survival rates depend on the patient’s underlying condition, age, and overall health. Many patients live for years after the surgery, but they may require lifelong monitoring of the prosthetic valve and the aorta.
9. What is the difference between the Bentall procedure and the David procedure?
While both procedures are aimed at treating aortic valve and aortic root conditions, the Bentall procedure involves replacing both the aortic valve and the ascending aorta with a prosthetic valve and conduit. In contrast, the David procedure (also known as aortic valve-sparing root replacement) attempts to preserve the patient’s native aortic valve while replacing only the aortic root and ascending aorta.
The David procedure may be preferred in younger patients with a healthy aortic valve to avoid the need for lifelong anticoagulation therapy.
10. Can patients with Marfan syndrome undergo the Bentall procedure?
Yes, patients with Marfan syndrome, which is a genetic disorder that affects connective tissue and leads to a higher risk of aortic aneurysm and dissection, are common candidates for the Bentall procedure. In these cases, the surgery is often performed early to prevent aortic rupture or severe valve dysfunction. The procedure may help reduce the risk of complications and improve long-term survival for these patients.
Conclusion
The Bentall procedure is a lifesaving operation requiring surgical precision, multidisciplinary coordination, and expert postoperative care. Understanding indications, contraindications, and alternative strategies is key to optimizing patient selection and improving long-term outcomes.
For more in-depth content on perfusion and cardiac surgery, visit Cardiperf.com!