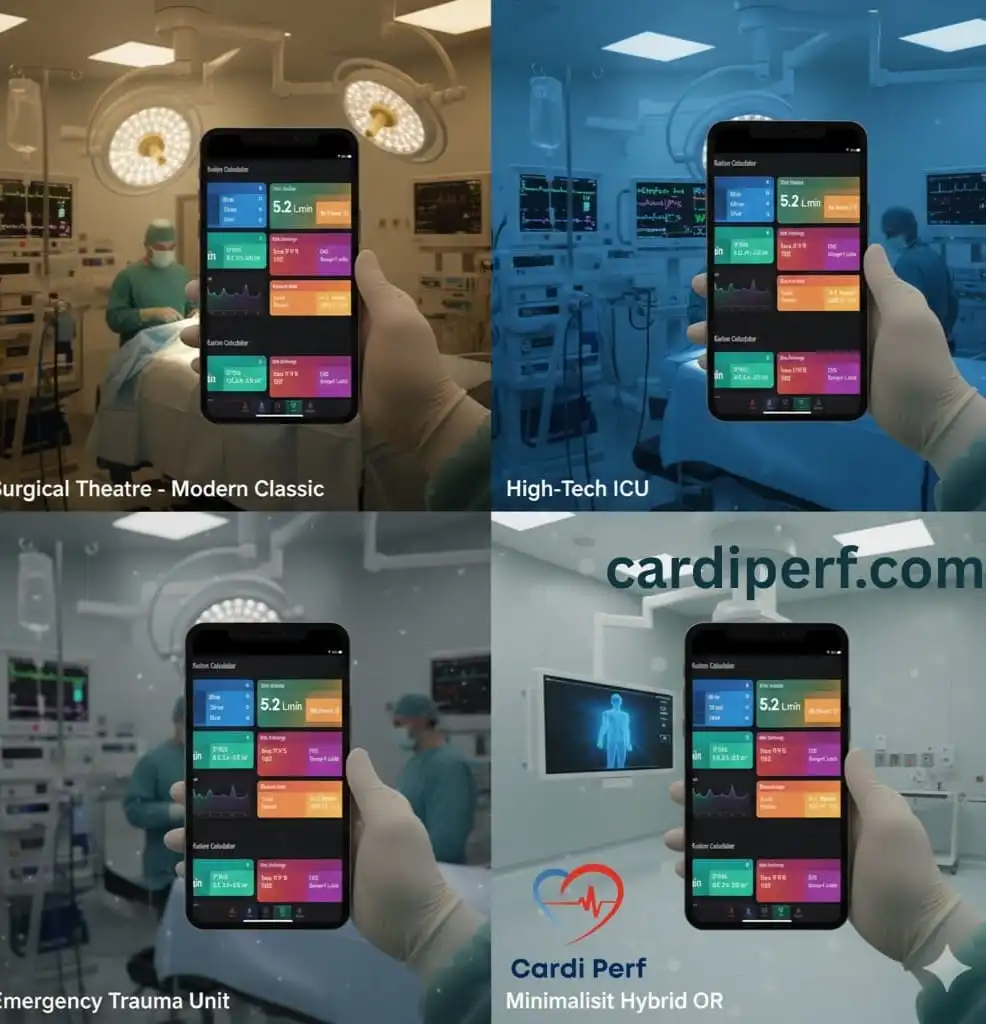
Advanced Perfusion Calculator
Clinical Edition – CPB Planning & Management
Advanced Parameters
Cannula Recommendations (Fr)
Additional Sizing Information
Blood Product Requirements
Anticoagulation Dosing
Oxygen Delivery Goals
Oxygenator Performance
Temperature Management
Perfusion Calculation Report
Generated on:
| Parameter | Value |
|---|---|
| BSA (Mosteller) | 0.00 m² |
| Target CPB Flow Rate | 0.00 L/min |
| Heparin Bolus | 0 Units |
| Projected DO2 Index | 0 mL/min/m² |
Of course. Here is a comprehensive explanation of a perfusion calculator, covering what it is, what it calculates, the underlying formulas, its critical applications, and its limitations.
What is a Perfusion Calculator?
A perfusion calculator is a clinical tool, often in the form of a software program, a mobile app, or a built-in function in a medical monitor, used to quantify blood flow to tissues and organs. It translates raw physiological data into meaningful numbers that help clinicians assess whether a patient’s vital organs are receiving adequate oxygen and nutrients.
At its core, perfusion is about the delivery of oxygenated blood to capillary beds in biological tissue. A perfusion calculator helps answer the fundamental clinical question: “Is this patient’s circulation sufficient to sustain their organs?”
Key Parameters Calculated
A comprehensive perfusion calculator doesn’t just compute one value. It integrates several key parameters to give a complete picture of the cardiovascular system’s performance.
1. Cardiac Output (CO) & Cardiac Index (CI)
This is the most fundamental measure of overall perfusion.
- Cardiac Output (CO): The volume of blood the heart pumps per minute.
- Formula:
CO = Heart Rate (HR) × Stroke Volume (SV) - Normal Range: 4-8 Liters/minute
- Formula:
- Cardiac Index (CI): A normalized version of CO that accounts for the patient’s body size, making it more useful for comparing individuals.
- Formula:
CI = Cardiac Output (CO) / Body Surface Area (BSA) - Normal Range: 2.5 – 4.0 L/min/m²
- BSA is often calculated using formulas like the Du Bois or Mosteller method.
- Formula:
2. Blood Pressure (BP) & Mean Arterial Pressure (MAP)
While a standard blood pressure is important, perfusion calculators focus on the average pressure driving blood through the systemic circulation.
- Mean Arterial Pressure (MAP): The average arterial pressure throughout one cardiac cycle. It is a critical determinant of coronary and cerebral perfusion.
- Formula (Estimated):
MAP ≈ Diastolic BP + 1/3(Systolic BP - Diastolic BP) - Example: For a BP of 120/80 mmHg,
MAP ≈ 80 + (1/3 * 40) = 93.3 mmHg. - Normal Range: 70-100 mmHg. A MAP of ≥ 65 mmHg is often a key target in shock management to ensure organ perfusion.
- Formula (Estimated):

3. Systemic Vascular Resistance (SVR) & Index (SVRI)
This measures the resistance (or “tightness”) the heart must pump against in the systemic circulation.
- Formula:
SVR = (MAP - CVP) / CO × 80- MAP: Mean Arterial Pressure
- CVP: Central Venous Pressure (the pressure in the great veins near the heart)
- CO: Cardiac Output
- 80: A conversion factor to metric units (Wood units → dyn·s·cm⁻⁵).
- SVRI: SVR indexed to BSA (
SVRI = SVR × BSA). - Interpretation:
- High SVR: Seen in hypovolemic or cardiogenic shock (vessels are constricted).
- Low SVR: Seen in septic or anaphylactic shock (vessels are dilated).
4. Oxygen Delivery (DO₂) & Consumption (VO₂)
These advanced parameters assess the purpose of perfusion: oxygen transport.
- Oxygen Delivery (DO₂): The total amount of oxygen delivered to the tissues per minute.
- Formula:
DO₂ = CO × Arterial Oxygen Content (CaO₂) CaO₂ = (Hgb × 1.34 × SaO₂) + (PaO₂ × 0.0031)- This shows that DO₂ depends on Cardiac Output, Hemoglobin (Hgb) level, and Oxygen Saturation (SaO₂).
- Formula:
- Oxygen Consumption (VO₂): The amount of oxygen consumed by the tissues per minute.
- Formula (Fick Principle):
VO₂ = CO × (CaO₂ - CvO₂) CvO₂is the oxygen content in mixed venous blood (from the pulmonary artery).
- Formula (Fick Principle):
5. Ejection Fraction (EF)
While primarily measured by echocardiogram, some advanced hemodynamic monitors can estimate it.
- Formula:
EF = (Stroke Volume / End-Diastolic Volume) × 100% - It represents the percentage of blood pumped out of the left ventricle with each contraction.
Clinical Applications: Where is it Used?
Perfusion calculations are vital in high-acuity medical settings:
- Intensive Care Units (ICU): For managing shock (septic, cardiogenic, hypovolemic), guiding fluid resuscitation, and titrating vasopressor/inotropic drugs (e.g., Norepinephrine, Dobutamine).
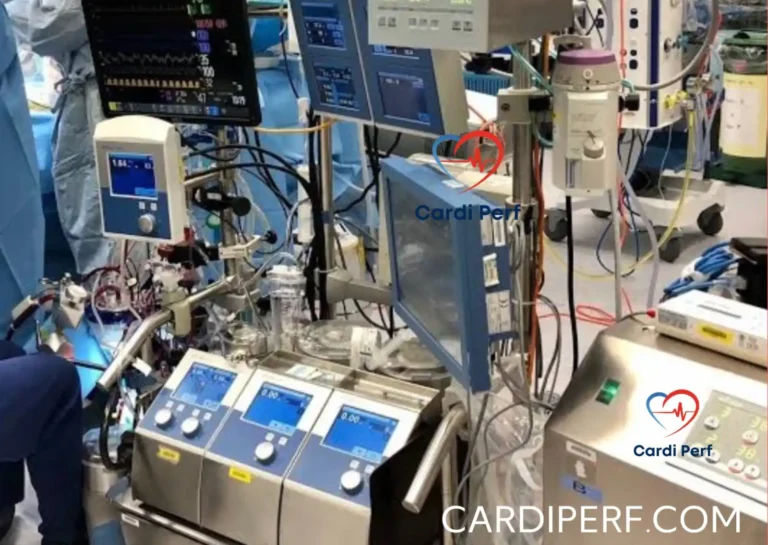
- Operating Rooms (OR): During major surgery, especially cardiac, vascular, and transplant surgeries, to ensure stable hemodynamics.
- Cardiology: To diagnose and monitor heart failure, assess the severity of valve diseases, and guide therapy.
- Emergency Medicine: In the rapid assessment and resuscitation of critically ill patients.
How are the Inputs Measured?
A perfusion calculator is only as good as its data. The inputs come from various monitors:
- Heart Rate (HR) & Blood Pressure (BP): Standard ECG and non-invasive or arterial line pressure monitoring.
- Stroke Volume (SV) & Cardiac Output (CO):
- Pulmonary Artery Catheter (PAC or Swan-Ganz): The historical gold standard, using thermodilution.
- Arterial Pulse Contour Analysis (e.g., PiCCO, FloTrac): Analyzes the shape of the arterial pressure waveform to estimate SV.
- Echocardiography (Ultrasound): Measures blood flow velocity and vessel diameter to calculate flow.
- Non-Invasive Cardiac Output Monitors (NICOM): Use bioreactance or other technologies.
- CVP: Measured via a central venous catheter.
- SaO₂ and PaO₂: From arterial blood gas (ABG) analysis.
- SvO₂/ScvO₂: Mixed venous oxygen saturation from a PAC, or central venous oxygen saturation from a central line.
Example Calculation Scenario
Situation: A 70kg man with sepsis. His BSA is 1.8 m².
Inputs:
- HR = 115 bpm
- SV (from monitor) = 50 mL
- MAP (from arterial line) = 55 mmHg
- CVP = 8 mmHg
- Hgb = 10 g/dL
- SaO₂ = 98%
Calculations:
- CO = HR × SV = 115 bpm × 0.05 L/beat = 5.75 L/min
- CI = CO / BSA = 5.75 / 1.8 = 3.2 L/min/m² (Low-normal, but the heart is tachycardic and compensating)
- SVR = (MAP – CVP) / CO × 80 = (55 – 8) / 5.75 × 80 = 654 dyn·s·cm⁻⁵ (Very low, indicating septic vasodilation)
- CaO₂ = (Hgb × 1.34 × SaO₂) + (PaO₂ × 0.0031) ≈ (10 × 1.34 × 0.98) ≈ 13.1 mL O₂/100 mL blood
- DO₂ = CO × CaO₂ × 10 = 5.75 L/min × 13.1 mL/dL × 10 = 753 mL O₂/min (May be inadequate for his metabolic demands).
Clinical Interpretation: The calculator reveals a classic septic shock picture: low blood pressure (low MAP) due to profoundly low systemic resistance (low SVR), with the heart working hard (high HR) to maintain a barely adequate cardiac output. The treatment would be fluids and vasopressors to increase the SVR and MAP.

Limitations and Pitfalls
- Garbage In, Garbage Out: Inaccurate input data (e.g., a dampened arterial line waveform) leads to meaningless calculations.
- Assumptions in Formulas: Many calculations, especially pulse contour analysis, rely on assumptions about vascular compliance which can change with disease, age, and medications.
- Snapshot in Time: Hemodynamics are dynamic. Calculations represent a single moment and must be interpreted in the context of trends.
- Not a Substitute for Clinical Judgment: A “normal” calculated number does not guarantee adequate tissue perfusion at the microcirculatory level. The clinician must always correlate these numbers with the patient’s overall condition, lactate levels, urine output, and mental status.
In summary, a perfusion calculator is an indispensable tool in modern critical care. It transforms complex physiological data into actionable insights, allowing clinicians to move beyond simple blood pressure readings and tailor life-supporting therapies with precision.