Potassium Level Calculator
Potassium in perfusion is one of the most critical factors that perfusionists must monitor to ensure patient safety and optimal outcomes during cardiopulmonary bypass (CPB).
For perfusionists, understanding the nuances of potassium physiology, its impact on myocardial function, and the best practices for its management is essential. This article delves into the importance of potassium, its role in cardiac function, and how to effectively monitor and manage it during CPB to ensure optimal patient outcomes.
What is Potassium? Why Potassium in Perfusion is Critical for Patient Safety and Why is it Important?
Potassium (K+) is a vital electrolyte that plays a central role in numerous physiological processes. It is the primary intracellular cation and is crucial for maintaining cellular homeostasis, nerve signaling, and muscle contraction.
Key Functions of Potassium : Best Practices for Potassium management in Perfusion During CPB:
- Cellular Homeostasis: Potassium regulates intracellular fluid volume, ensuring proper osmotic balance.
- Nerve Function: It is essential for generating and propagating action potentials in neurons.
- Muscle Contraction: Potassium facilitates the contraction and relaxation of skeletal and cardiac muscles.
- Acid-Base Balance: It participates in buffering systems that maintain the body’s pH equilibrium.
- Renal Regulation: Potassium excretion is primarily controlled by the kidneys, influenced by hormones like aldosterone and renin.
Why Potassium is Critical in Cardiac Surgery:
- Cardiac Rhythm: Potassium is essential for maintaining the heart’s electrical activity.
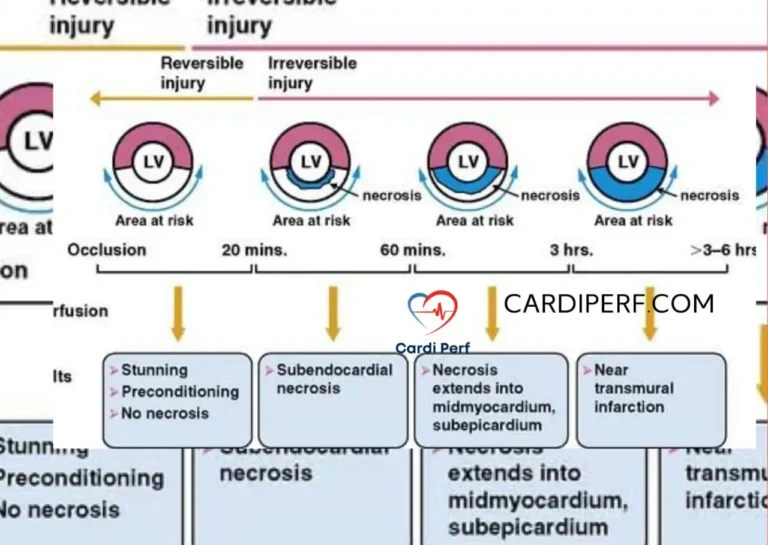
- Myocardial Protection: Proper potassium levels are crucial during CPB to protect the heart from ischemic injury.
- Hemodynamic Stability: Imbalances can lead to severe complications, including arrhythmias and cardiac arrest.
Potassium’s Role in Cardiac Function
Potassium is indispensable for cardiac electrophysiology. It helps maintain the resting membrane potential and facilitates the repolarization phase of the cardiac action potential.
Key Roles of Potassium in the Heart:
- Resting Membrane Potential: Potassium establishes a negative intracellular charge, which is necessary for electrical stability.
- Repolarization: It ensures proper resetting of myocardial cells after each contraction.
- Excitability: Potassium levels influence the heart’s ability to respond to electrical stimuli.
- Rhythmicity: Stable potassium levels help maintain regular sinus rhythm and prevent arrhythmias.
- Cardiac Contractility: Potassium modulates the strength of myocardial contractions by affecting ion channel activity.

Consequences of Potassium Imbalance:
- Hypokalemia (Low Potassium): Can cause arrhythmias, muscle weakness, and cardiac arrest.
- Hyperkalemia (High Potassium): Can lead to bradycardia, ventricular fibrillation, and asystole.
Potassium and Cardiopulmonary Bypass (CPB)
CPB is a complex procedure that can significantly impact potassium levels. Understanding these changes is crucial for effective management.
How CPB Affects Potassium Levels:
- Hemodilution: The use of priming solutions can dilute potassium, leading to hypokalemia.
- Hypothermia: Low temperatures during CPB can cause intracellular potassium shifts, reducing serum levels.
- Cardioplegia Solutions: Potassium-rich cardioplegia can cause hyperkalemia during reperfusion.
- Insulin Administration: Insulin drives potassium into cells, potentially causing hypokalemia.
Challenges in Potassium Management During CPB:
- Rapid shifts in potassium levels can destabilize cardiac function.
- Frequent monitoring and adjustments are required to maintain optimal levels.
Hypokalemia: Causes, Risks, and Management
Hypokalemia, or low potassium levels, is a common concern during CPB. It can lead to severe complications if not promptly addressed.
Causes of Hypokalemia During CPB:
- Hemodilution from priming solutions
- Hypothermia-induced intracellular shifts
- Diuretic use
- Insulin administration
Risks of Hypokalemia:
- Arrhythmias (e.g., ventricular tachycardia, fibrillation)
- Muscle weakness and paralysis
- Impaired myocardial contractility
Management Strategies:
- Potassium Replacement: Gradual IV supplementation (10-20 mmol/hour) to avoid rapid shifts.
- Monitoring: Frequent arterial blood gas (ABG) analysis to track potassium levels.
- Adjusting CPB Prime: Modifying the composition of priming solutions to minimize dilutional effects.
Potassium Replacement Formula for Hypokalemia:
To calculate the potassium deficit and replacement dose:
- Determine the Potassium Deficit:
Potassium Deficit (Kdeficit in mmol) = (Knormal lower limit − Kmeasured) × kg body weight × 0.3.
In adult , the calculated deficit would be (4.0 − 3.3) × 75 × 0.3, or 15 mmol.
while in children , the calculated deficit would be (3.5 − 2.3) × 20 × 0.3, or 7.2 mmol.
- Desired K+: Typically 4.0 – 4.5 mmol/L
- Current K+: Measured serum potassium level
- Weight: Patient’s weight in kilograms
- 0.3: Represents the distribution factor for potassium (30% extracellular fluid)
- Administer Replacement:
- Replace 50% of the calculated deficit initially.
- Recheck potassium levels after 1-2 hours and adjust as needed.
- Avoid exceeding 20 mmol/hour to prevent rapid shifts and arrhythmias.
Hyperkalemia: Causes, Risks, and Management
Hyperkalemia, or high potassium levels, is another critical concern during and after CPB.
Causes of Hyperkalemia During CPB:
- Potassium-rich cardioplegia solutions
- Reperfusion injury releasing intracellular potassium
- Impaired renal function
Risks of Hyperkalemia:
- Bradycardia
- Ventricular fibrillation
- Cardiac arrest
Management Strategies:
- Calcium Administration: Stabilizes the cardiac membrane and reduces arrhythmia risk.
- Insulin and Glucose: Drives potassium into cells, lowering serum levels.
- Potassium-Binding Agents: Used in severe cases to remove excess potassium.
Correction Formula for Hyperkalemia:
- Calcium Gluconate (10%):
- Dose: 10 mL IV over 2-5 minutes.
- Effect: Stabilizes the cardiac membrane within minutes.
- Insulin and Glucose:
- Dose: 10 units of regular insulin IV with 25-50 grams of glucose (e.g., 50 mL of 50% dextrose).
- Effect: Shifts potassium into cells, lowering serum levels within 15-30 minutes.
- Sodium Bicarbonate:
- Dose: 50-100 mEq IV over 5-10 minutes.
- Effect: Alkalizes blood, driving potassium into cells.
- Potassium-Binding Agents:
- Sodium Polystyrene Sulfonate (Kayexalate): 15-30 g orally or rectally.
- Patiromer: 8.4-16.8 g orally.
Potassium Monitoring Techniques in Perfusion
Accurate monitoring of potassium levels is essential for effective management during CPB.
Common Monitoring Methods:
- Arterial Blood Gas (ABG) Analysis: Provides real-time potassium levels.
- Serum Electrolyte Panels: Regular blood tests to track potassium and other electrolytes.
- Continuous Monitoring Systems: Advanced technologies for real-time tracking during surgery.
Best Practices for Monitoring Electrolyte balance in cardiac surgery:
- Frequent sampling during critical phases of CPB.
- Correlating potassium levels with clinical symptoms and hemodynamic status.
Optimal Potassium Levels During CPB
Maintaining optimal potassium levels is crucial for myocardial protection and hemodynamic stability.
Recommended Potassium Levels:
- Normal Range: 3.5 – 5.0 mmol/L
- During CPB: Slightly elevated levels (4.0 – 5.5 mmol/L) may be maintained to optimize myocardial protection.
Factors Influencing Optimal Levels:
- Patient’s baseline potassium levels
- Type and duration of surgery
- Use of cardioplegia solutions
Potassium Replacement Strategies
Effective potassium replacement is key to managing hypokalemia during CPB.
Guidelines for Potassium Replacement:
- Dosage: 10-20 mmol/hour, adjusted based on ABG results.
- Route: IV administration for rapid effect.
- Monitoring: Frequent ABG analysis to avoid overcorrection.
Risks of Overcorrection:
- Rapid shifts can cause arrhythmias and cardiac instability.
Potassium-Binding Agents and Their Use in Perfusion
Potassium-binding agents are used to manage severe hyperkalemia.
Common Agents:
- Sodium Polystyrene Sulfonate (Kayexalate): Binds potassium in the gut.
- Patiromer: A newer agent with fewer side effects.
Indications for Use:
- Severe hyperkalemia unresponsive to other treatments.
- Postoperative hyperkalemia due to renal impairment.

Case Studies on Potassium Management in Perfusion
Real-world examples highlight the importance of effective potassium management.
Case Study 1: Hypokalemia During CPB
- Patient Presentation: A 65-year-old male undergoing CABG developed hypokalemia during CPB.
- Intervention: Gradual potassium replacement and adjustment of priming solutions.
- Outcome: Successful stabilization of potassium levels and uneventful recovery.
Case Study 2: Hyperkalemia Post-CPB
- Patient Presentation: A 70-year-old female developed hyperkalemia after aortic valve replacement.
- Intervention: Calcium, insulin, and glucose administration.
- Outcome: Potassium levels normalized, and the patient recovered without complications.
Common Myths About Potassium in Perfusion
Misconceptions about potassium management can lead to suboptimal care.
Myth 1: Rapid Potassium Correction is Safe
- Fact: Rapid correction can cause arrhythmias and should be avoided.
Myth 2: Hyperkalemia is Always Due to Renal Failure
- Fact: Hyperkalemia can result from multiple factors, including reperfusion injury and cardioplegia.
FAQs
1. What is the normal range for potassium in cardiac surgery patients?
The normal potassium range is 3.5 – 5.0 mmol/L; however, during cardiac procedures, a slightly elevated range (4.0 – 5.5 mmol/L) may be maintained to optimize myocardial protection.
2. How does CPB affect potassium levels?
CPB can cause hypokalemia due to hemodilution, hypothermia-induced intracellular shifts, and insulin administration. Conversely, potassium-containing cardioplegia solutions can lead to hyperkalemia.
3. What is the safest way to correct hypokalemia during CPB?
Gradual IV potassium supplementation (not exceeding 10-20 mmol/hour) is recommended to prevent rapid shifts and associated arrhythmias.
4. Why does hyperkalemia occur postoperatively?
Hyperkalemia after CPB may result from impaired renal function, cellular reperfusion injury, or residual potassium-rich cardioplegia.
5. What interventions help prevent potassium imbalances during surgery?
- Frequent electrolyte monitoring via ABG analysis
- Adjusting CPB prime composition
- Controlled administration of diuretics, insulin, and calcium
6. Can potassium imbalance cause complications beyond arrhythmias?
Yes, severe potassium imbalances Hypokalemia and hyperkalemia in perfusion can lead to muscle weakness, paralysis, metabolic disturbances, and multi-organ dysfunction.
Conclusion
Potassium in perfusion plays a vital role in ensuring patient safety and optimizing outcomes during cardiac surgery. Effective potassium management is essential for ensuring patient safety and optimizing cardiac function during CPB. By understanding potassium physiology, monitoring fluctuations, and applying targeted interventions, perfusionists can enhance surgical outcomes and improve patient care.
References
- Smith, J. et al. (2020). Potassium Management in Cardiac Surgery. Journal of Perfusion Science.
- Brown, A. et al. (2019). Electrolyte Imbalances During CPB. Cardiac Surgery Today.
- National Institutes of Health (NIH). (2021). Potassium and Heart Health.
This comprehensive guide provides healthcare providers with actionable insights into potassium management during CPB, ensuring better patient outcomes and enhanced clinical practice.