Table of Contents
- Introduction
- Understanding Blood Pressure and Cardiac Output
- 2.1 What is Blood Pressure?
- 2.1 What is Cardiac Output?
- The Importance of Blood Pressure Regulation in Perfusion
- 3.1 Impact on Organ Perfusion
- 3.2 Strategies for Blood Pressure Control in Cardiac Surgery
- Cardiac Output and Its Relevance to Cardiac perfusion professionals
- 4.1 How Cardiac Output Affects Oxygen Delivery
- 4.2 Managing Cardiac Output During Bypass and ECMO
- Key Factors Influencing Blood Pressure and Cardiac Output
- 5.1 Preload, Afterload, and Contractility
- 5.2 The Role of Drugs in Managing Blood Pressure and Cardiac Output
- 5.3 Frequently Used Medications for BP and Cardiac Output Management
- Practical Tips for Cardiac perfusion professionals in Managing Blood Pressure and Cardiac Output
- Conclusion
- Frequently Asked Questions (FAQs)
Introduction
For perfusionists, mastering blood pressure regulation and cardiac output management is essential to optimizing patient outcomes in high-risk procedures like cardiac surgery and ECMO. Understanding the complex relationship between hemodynamic stability and cardiac output is essential for ensuring optimal patient care during cardiac surgery and other perfusion interventions. These two critical hemodynamic parameters—blood pressure regulation and cardiac output management—play a significant role in the success of high-stakes procedures such as ECMO, cardiac bypass, and organ perfusion. In this article, we will delve into why effective blood pressure regulation and precise management of cardiac output are indispensable for perfusionists, and how a deeper understanding of these concepts can significantly improve clinical decision-making in critical surgical and perfusion interventions.
Understanding Blood Pressure and Cardiac Output
What is Blood Pressure?
Blood pressure (BP) refers to the force of blood against the walls of the arteries as the heart pumps blood through the body. It is measured in millimeters of mercury (mmHg) and consists of two components:
- Systolic Blood Pressure (SBP): The pressure when the heart contracts and pumps blood into the arteries.
- Diastolic Blood Pressure (DBP): The pressure when the heart is at rest between beats.
The regulation of BP is crucial, as it determines the perfusion of vital organs and tissues. Low BP can lead to hypoperfusion, while high BP may damage blood vessels and organs.
What is Cardiac Output?
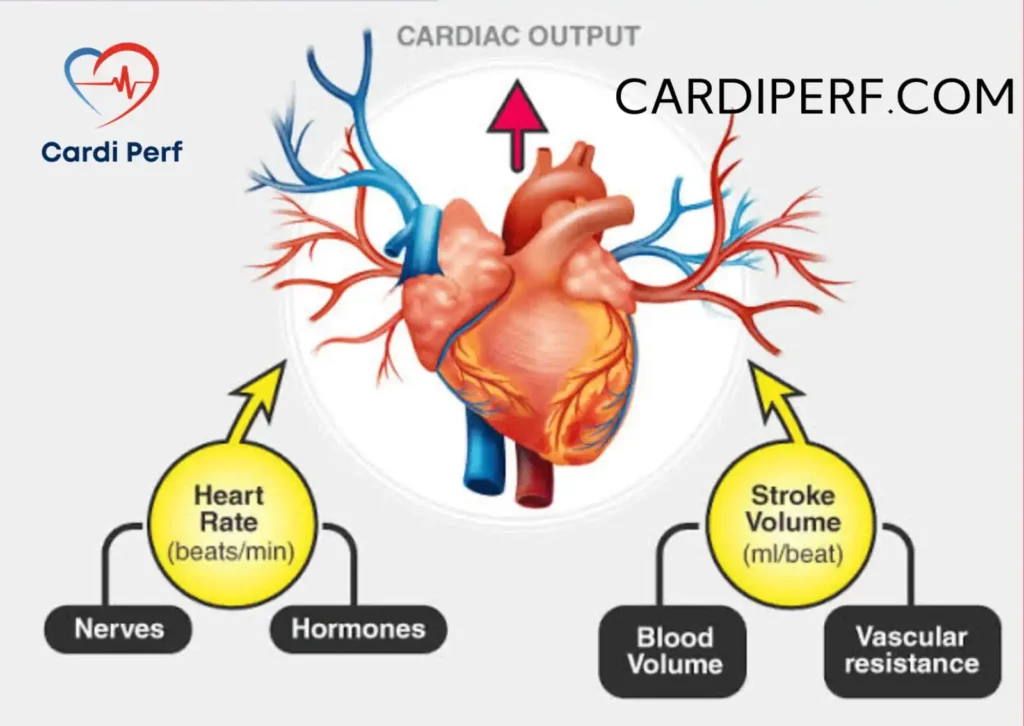
Cardiac Output (CO) refers to the volume of blood the heart pumps per minute, and it is calculated by multiplying heart rate (HR) and stroke volume (SV):
- CO = HR × SV
A healthy CO is necessary to meet the metabolic demands of tissues, especially the brain, kidneys, and heart itself. CO is influenced by several factors, including preload, afterload, contractility, and vascular resistance.
The Importance of Blood Pressure Regulation in Perfusion
Impact on Organ Perfusion
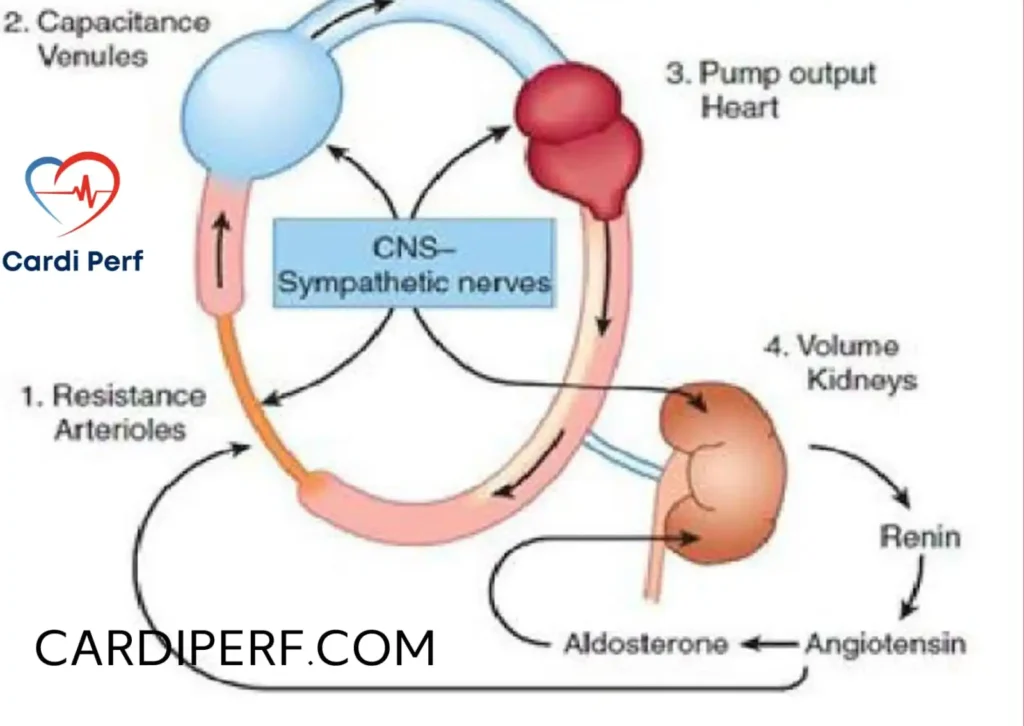
For perfusionists, one of the primary goals is to maintain adequate perfusion pressure to ensure the delivery of oxygen and nutrients to tissues. Low blood pressure can compromise organ perfusion, especially in patients undergoing surgery or on circulatory support devices like ECMO. Organs such as the brain and kidneys are particularly vulnerable to ischemia from inadequate perfusion, leading to organ failure.
Conversely, high blood pressure can damage delicate blood vessels and compromise tissue oxygenation. Therefore, carefully managing blood pressure during surgeries, including using vasopressors or vasodilators, is vital for maintaining hemodynamic stability and improving patient outcomes.
How to Monitor Cardiac Output and Ensure Blood Pressure Control
Cardiac perfusion professionals often need to regulate blood pressure in real-time during cardiac surgeries. This can include:
- Adjusting perfusion flow rates: Optimizing blood flow to match the patient’s physiological needs.
- Utilizing medications: Administering drugs like vasopressors, vasodilators, or inotropes to control BP and improve circulation.
- Monitoring for hypotension: Ensuring adequate perfusion to vital organs, particularly during phases like hypothermic circulatory arrest or cardioplegia.
Cardiac Output and Its Relevance to Perfusionists
How Cardiac Output Affects Oxygen Delivery
Cardiac output is a direct indicator of the heart’s ability to meet the body’s oxygen demands. In the context of perfusion, a low CO indicates insufficient blood flow, which can lead to inadequate oxygen delivery to tissues, increasing the risk of organ damage and hypoxia. Perfusionists must be vigilant about maintaining optimal CO during cardiac surgery, ECMO, and cardiopulmonary bypass.
Managing Cardiac Output During Bypass and ECMO
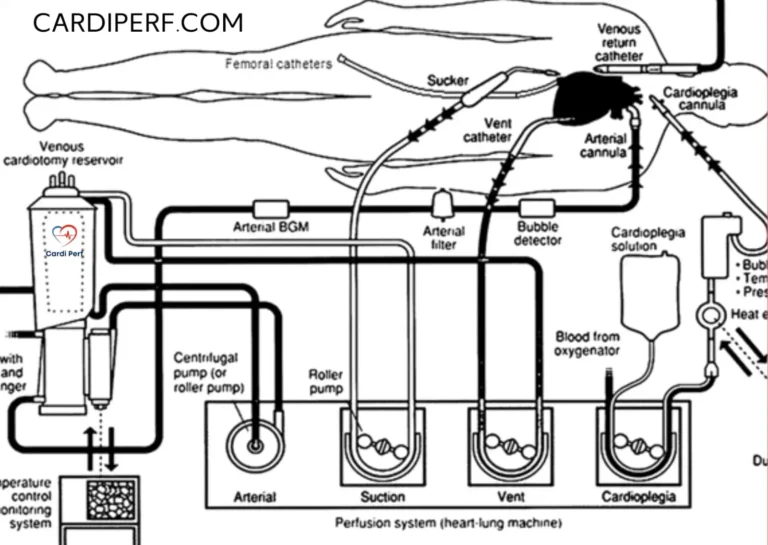
In procedures like cardiopulmonary bypass (CPB) and ECMO, where the heart is temporarily bypassed, managing CO becomes even more critical. Perfusionists must adjust the pump flow rates to ensure that the patient’s organs receive adequate oxygenation and perfusion. This includes:
- Monitoring pump flow: Ensuring the bypass pump is providing an adequate flow to mimic physiological circulation.
- Adjusting oxygenator settings: Tailoring oxygenation levels to the patient’s needs to avoid hypoxemia.
- Managing afterload and preload: These parameters directly impact CO and must be optimized using fluid management and vasopressor interventions.
Several factors, including preload, afterload, and contractility, influence BP regulation and cardiac output, which perfusionists need to monitor during surgery.
Preload, Afterload, and Contractility
Perfusionists must understand how preload, afterload, and contractility affect both BP and CO. Here’s a quick rundown:
- Preload: The volume of blood entering the heart before contraction. Increased preload can increase CO, but excessive preload may strain the heart.
- Afterload: The resistance the heart must overcome to eject blood. High afterload can reduce CO and increase workload on the heart.
- Contractility: The force of the heart’s contraction. Poor contractility reduces CO and is a key consideration when managing heart failure or during cardioplegia.
The Role of Drugs in Managing Blood Pressure and Cardiac Output
Pharmacological interventions are often required to manage BP and CO during surgery. Here’s a list of frequently used drugs and their role in managing blood pressure and cardiac output:
- Norepinephrine
- Use: Vasopressor for managing hypotension. It increases systemic vascular resistance and raises blood pressure by constricting blood vessels.
- Dosage: Typically administered intravenously. Adjusted to maintain MAP (mean arterial pressure) of 60–65 mmHg in most cases.
- Epinephrine
- Use: A potent vasopressor and inotropic agent. It increases both heart rate and contractility, making it useful for cardiac arrest and septic shock.
- Dosage: Infusion rate varies based on the clinical situation, often between 0.01–0.5 mcg/kg/min.
- Phenylephrine
- Use: Selective alpha-1 adrenergic agonist. Increases blood pressure by constricting arterioles. Commonly used in postoperative hypotension.
- Dosage: Administered via IV, starting at a rate of 40 mcg/min and titrated based on BP response.
- Nitroglycerin
- Use: Vasodilator used to reduce afterload and treat hypertension. It is particularly useful for controlling pulmonary hypertension or managing left ventricular failure.
- Dosage: Administered intravenously, beginning at 5 mcg/min and adjusted based on BP and clinical response.
- Milrinone
- Use: A phosphodiesterase inhibitor that increases contractility and cardiac output. Used in heart failure and ECMO patients to improve myocardial performance.
- Dosage: Typical IV infusion starts at 0.375–0.75 mcg/kg/min.
- Dobutamine
- Use: Inotropic agent that improves cardiac output and contractility. Frequently used during cardiac surgery and for managing acute heart failure.
- Dosage: Typically given as an infusion starting at 2.5 mcg/kg/min.
- Labetalol
- Use: Beta-blocker and alpha-blocker combination. It reduces both heart rate and blood pressure, making it useful in managing hypertension during cardiac surgery.
- Dosage: IV administration, usually starting at 5 mg and titrating every 10 minutes, up to 20 mg.
- Vasopressin
- Use: Antidiuretic hormone that increases vascular tone and raises blood pressure. Often used in cases of septic shock and cardiogenic shock.
- Dosage: IV infusion starting at 0.01–0.04 units/min.
- Isoproterenol
- Use: A beta-agonist that increases heart rate and myocardial contractility. Used in situations of bradycardia and to stimulate the sinoatrial node.
- Dosage: IV infusion, starting at 1 mcg/min and titrated based on heart rate response.
- Sodium Nitroprusside
- Use: A powerful vasodilator used to reduce blood pressure rapidly in cases of hypertensive crisis.
- Dosage: IV infusion starting at 0.3 mcg/kg/min.
Practical Tips for Perfusionists in Managing Blood Pressure and Cardiac Output
As a perfusionist, you must master the following strategies for managing BP and CO:
- Frequent Monitoring: Use continuous monitoring tools to assess BP, CO, and other hemodynamic parameters throughout the procedure.
- Adjust Flow Rates and Settings: Regularly tweak the flow rates of the bypass machine, ECMO, or oxygenator to match the patient’s changing needs.
- Collaborate with the Surgical Team: Work closely with the cardiac surgical team to manage medications, fluid balance, and mechanical support to maintain stable hemodynamics.
Frequently Asked Questions (FAQs)
- What is the normal range for blood pressure in a perfusion patient?
- The ideal blood pressure range varies by patient, but a common target during cardiac surgery is around 90-120/60-80 mmHg.
- How does low cardiac output affect patient recovery?
- Low cardiac output can lead to organ ischemia and hypoxia, delaying recovery and increasing the risk of organ failure.
- What are the risks of high blood pressure during cardiac surgery?
- High blood pressure during cardiac surgery can cause vascular damage, increase bleeding risk, and compromise organ perfusion.
- What is the role of ECMO in managing cardiac output?
- ECMO provides temporary cardiac and/or respiratory support when the heart is unable to maintain adequate output, helping maintain tissue perfusion.
- How do vasopressors help manage blood pressure?
- Vasopressors like norepinephrine and epinephrine constrict blood vessels, raising systemic vascular resistance and increasing BP.
- Why is monitoring cardiac output so important during perfusion?
- Monitoring CO helps ensure that oxygenated blood reaches vital organs, preventing ischemia and supporting the patient’s overall metabolism.
- Can perfusionists adjust blood pressure medications during surgery?
- Yes, perfusionists often collaborate with the surgical team to adjust blood pressure medications based on the patient’s hemodynamics.
- Why is cardiac output management essential during ECMO?
- During ECMO, BP can be managed through appropriate fluid management, medications (vasopressors or vasodilators), and adjusting the ECMO pump flow rate.
- What medications should be avoided during cardiac surgery?
- Some medications like NSAIDs (e.g., ibuprofen) should be avoided pre-surgery due to their anticoagulant effects, which may increase bleeding risk.
- How does afterload affect cardiac output?
- Increased afterload (resistance) makes it harder for the heart to eject blood, which can reduce cardiac output and impact perfusion.
Conclusion
.Mastering blood pressure regulation and cardiac output is indispensable for perfusionists aiming to ensure the best possible patient outcomes during critical cardiac interventions. BP regulation and cardiac output management are two of the most crucial aspects of a perfusionist’s role. By understanding the physiological mechanisms behind BP and CO, perfusionists can make informed decisions during critical procedures, such as cardiac surgery, ECMO, and CPB, ensuring optimal patient outcomes. Mastering these concepts is essential for any perfusion professional, as they directly impact organ perfusion, oxygen delivery, and the overall success of the procedure. For update are current issues visit us at cardiperf.com