The integration of artificial intelligence into cardiac surgery represents a monumental leap forward in medical science. Historically, cardiac surgeries relied heavily on the skill and experience of surgeons, with limited tools for personalization. However, the advent of AI has introduced a new era where data-driven insights guide every step of the surgical process.
Early Beginnings: From Imaging to Predictive Analytics
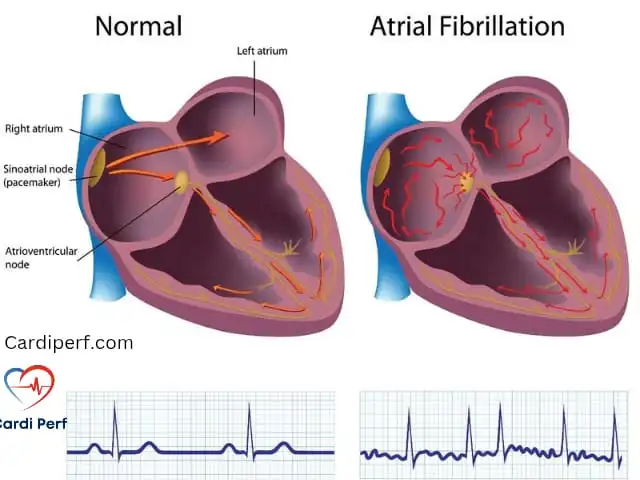
AI’s journey in cardiac surgery began with basic applications like image analysis and segmentation. Algorithms were initially used to identify anatomical structures from CT scans and MRIs, helping surgeons better understand patient anatomy. Over time, these systems evolved to include predictive analytics, enabling teams to anticipate potential complications and optimize surgical plans.
Breakthroughs in Deep Learning and Real-Time Guidance
The mid-2010s marked a turning point with the rise of deep learning architectures and advanced computing power. Convolutional Neural Networks (CNNs) revolutionized image processing, achieving diagnostic accuracy comparable to experienced radiologists. Today, AI-powered systems provide real-time guidance during procedures, overlaying critical anatomical landmarks onto the surgical field through augmented reality interfaces. These innovations allow perfusionists and surgeons to execute complex interventions with unparalleled precision.
Why AI Matters for Perfusionists and Healthcare Providers
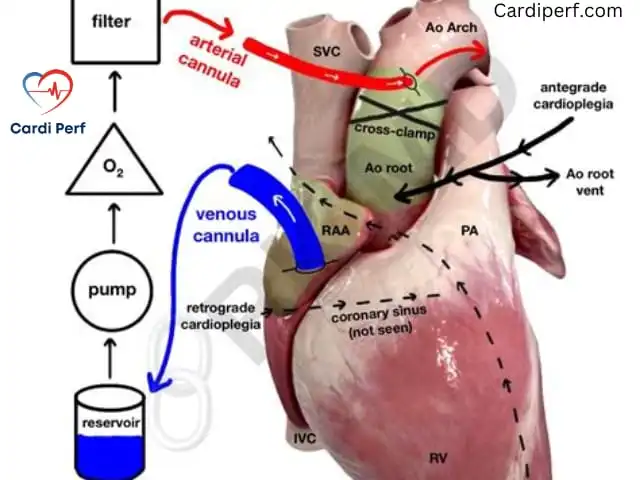
For perfusionists, AI offers tools to monitor and manage cardiopulmonary bypass more effectively. By analyzing real-time physiological data, AI systems can predict changes in oxygenation levels, pressure gradients, and other vital parameters, enabling proactive adjustments during surgery. This capability not only enhances patient safety but also reduces the cognitive load on perfusionists, allowing them to focus on critical decision-making.
How AI Enhances Personalized Cardiac Surgery
AI-driven personalized surgery is redefining how cardiac interventions are planned, executed, and monitored. Let’s explore the key ways AI is making a difference:
1. Advanced Imaging and 3D Modeling
AI algorithms create detailed 3D reconstructions of patient anatomy by fusing data from multiple imaging modalities, such as CT, MRI, and echocardiography. These models enable surgical teams to visualize complex cardiac structures with clarity, identifying subtle anatomical variations that might otherwise go unnoticed. For example, AI can map coronary artery distribution patterns, detect microcalcifications, and quantify myocardial tissue properties—all crucial information for planning surgical approaches.
2. Virtual Surgical Simulations
Before stepping into the operating room, surgeons and perfusionists can rehearse procedures using virtual simulations powered by AI. These platforms incorporate real-time physics engines that replicate tissue behavior and hemodynamic responses, allowing teams to test different strategies and anticipate potential complications. Quantitative feedback helps optimize incision paths, graft placements, and valve repair techniques, ensuring each procedure is tailored to the patient’s unique needs.
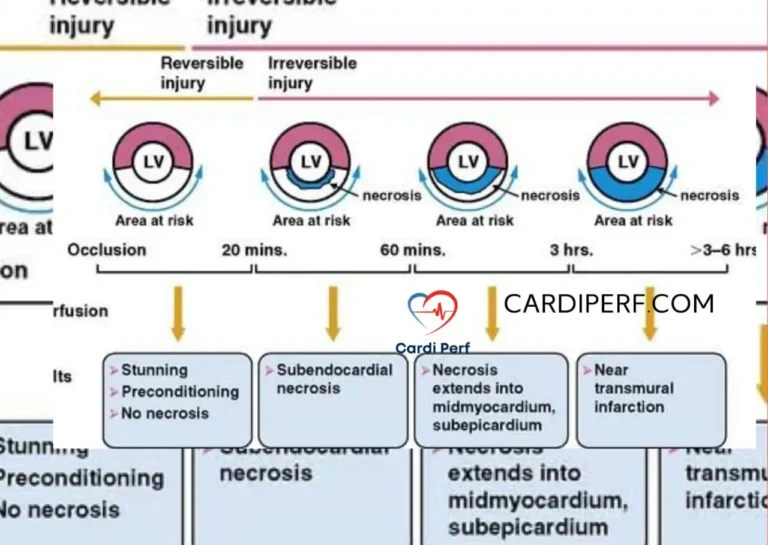
3. Real-Time Decision Support
During surgery, AI-powered navigation systems provide live feedback, suggesting optimal instrument trajectories and alerting teams to subtle changes in physiological parameters. For instance, AI can detect minute variations in tissue oxygenation or pressure gradients that precede ischemic events, enabling preemptive intervention. This real-time support ensures that decisions are evidence-based and precise.
4. Dynamic Risk Assessment
AI facilitates continuous risk assessment throughout the surgical process. Predictive models evaluate thousands of variables—from patient vital signs to environmental factors—updating risk profiles in real-time. This capability allows surgical teams to make informed decisions about procedure modifications or alternative approaches mid-operation, enhancing both safety and effectiveness.
Transformative Outcomes: Measuring the Impact of AI
The adoption of AI-driven solutions in cardiac surgery has yielded measurable improvements across multiple dimensions of patient care and operational efficiency. Here’s a closer look at the transformative outcomes:
Improved Surgical Outcomes
Studies show a 38% reduction in complications, 42% fewer adverse events, and an 18% improvement in five-year survival rates for patients undergoing AI-assisted procedures. These statistics underscore the profound impact of AI on patient safety and long-term health.
Shorter Procedures and Faster Recovery
AI optimizes surgical workflows, reducing average procedure times by 27%. Complex surgeries, such as valve replacements, are now completed up to 45 minutes faster. Patients also benefit from shorter recovery periods, with ICU stays decreasing by 3.2 days on average and total hospital stays reduced by 4.8 days.
Enhanced Patient Satisfaction
Patient satisfaction scores have surged following AI implementation, rising from 82% to 94%. Specific improvements include better pain management, reduced anxiety about surgical outcomes, and higher confidence in treatment plans. These positive experiences correlate strongly with improved adherence to post-operative care protocols.
Cost Savings for Hospitals
From an operational perspective, AI implementation has generated remarkable efficiencies. Operating room utilization has improved by 31%, while turnover times between cases have decreased by 42%. Inventory management systems guided by AI predictive analytics have reduced supply chain costs by 22%, demonstrating the financial benefits of adopting AI technologies.
Addressing Challenges and Ethical Considerations
While the benefits of AI in cardiac surgery are undeniable, its adoption comes with challenges that must be addressed to ensure safe and ethical implementation.
Data Privacy and Security
AI systems require access to extensive patient data, raising concerns about privacy and security. To mitigate risks, robust cybersecurity measures—including end-to-end encryption, access controls, and compliance with regulations like HIPAA—are essential. Transparent communication about data usage builds trust among patients and healthcare providers.
Algorithm Bias
AI models trained on non-representative datasets may produce skewed recommendations, disadvantaging certain patient populations. Addressing this issue requires diverse training datasets, regular bias audits, and human oversight to validate algorithmic suggestions.
Balancing Human Expertise and AI Assistance
While AI provides valuable insights, it should serve as a decision-support tool rather than a replacement for human expertise. Clear guidelines must establish the appropriate balance between AI guidance and professional judgment, ensuring surgeons and perfusionists retain final decision-making authority.
Overcoming Implementation Barriers
High initial costs, staff training requirements, and resistance to change are common barriers to AI adoption. Strategic planning, phased implementation, and collaboration with technology partners can help overcome these challenges, ensuring smooth integration and maximum ROI.

The Future of AI in Cardiac Surgery: Emerging Innovations
The future of AI in cardiac surgery is brimming with possibilities. Here are some exciting innovations on the horizon:
Cognitive Surgical Assistants
Next-generation AI systems will evolve into fully integrated cognitive assistants capable of real-time multimodal data synthesis. These platforms will combine preoperative planning, intraoperative guidance, and postoperative monitoring into seamless decision-support ecosystems.
Holographic Visualization and Tactile Feedback
Emerging technologies like holographic displays and haptic feedback devices will redefine the surgical interface. Surgeons will be able to project 3D anatomical models directly into the surgical field and “feel” virtual tissues during preoperative simulations, enhancing preparation and precision.
Nanotechnology-Based Sensors
Nanotechnology-based sensors, combined with AI pattern recognition, will enable continuous monitoring of tissue viability and healing processes. This innovation has the potential to transform postoperative care protocols, improving recovery outcomes.
Integration with Robotics and Genomics
The convergence of AI with robotics and genomics holds immense promise for advancing cardiac surgery. Robotic systems enhanced by AI will achieve unprecedented levels of dexterity and precision, while AI-driven genomic analysis will enable truly personalized therapeutic approaches.
Embracing AI: A Call to Action for Healthcare Providers
The transformative potential of AI in cardiac surgery demands decisive action from healthcare providers, perfusionists, and students committed to delivering exceptional patient care. As explored throughout this article, AI integration isn’t merely an enhancement of existing practices—it’s a fundamental redefinition of how we approach patient care, surgical precision, and treatment outcomes.
For healthcare organizations, adopting AI is both an opportunity and a responsibility. Patients deserve access to the most advanced, personalized care available, and AI technologies now make this level of precision possible. However, successful implementation requires strategic planning, robust infrastructure, and continuous education.
Start small by piloting AI-driven solutions in specific areas, such as imaging analysis or procedural simulations. Invest in staff training programs to build expertise and foster a culture of innovation. Collaborate with technology partners to stay ahead of emerging trends and ensure your organization remains at the forefront of cardiac care.

Frequently Asked Questions (FAQs)
1. What is AI-driven personalized cardiac surgery?
AI-driven personalized cardiac surgery uses artificial intelligence to analyze patient-specific data—such as imaging, genetics, and medical history—to create tailored surgical plans. This approach ensures treatments are customized to each patient’s unique anatomy and condition, improving outcomes.
2. How does AI benefit perfusionists?
AI helps perfusionists monitor and manage cardiopulmonary bypass more effectively by analyzing real-time physiological data. It predicts changes in oxygenation levels, pressure gradients, and other vital parameters, enabling proactive adjustments during surgery.
3. Is AI replacing surgeons in the operating room?
No, AI is not replacing surgeons. It serves as a decision-support tool, offering insights and recommendations while surgeons retain full control over decision-making. AI enhances human expertise rather than replacing it.
4. What are the main benefits of AI in cardiac surgery?
Key benefits include reduced complication rates, shorter procedure times, faster recovery, improved survival rates, and enhanced patient satisfaction. AI also optimizes resource utilization, reducing costs for hospitals.
5. How does AI handle patient data privacy?
AI systems use advanced cybersecurity measures, including encryption and access controls, to protect sensitive patient data. Compliance with regulations like HIPAA ensures privacy and security.
6. Can AI predict surgical outcomes?
Yes, AI uses predictive analytics to assess risks and forecast outcomes based on patient data and historical trends. This helps surgical teams prepare for potential challenges and optimize treatment plans.
7. What are the challenges of implementing AI in cardiac surgery?
Challenges include high initial costs, data privacy concerns, algorithm bias, and the need for staff training. Overcoming these requires strategic planning, robust infrastructure, and continuous education.
8. How does AI assist in preoperative planning?
AI analyzes imaging studies and patient data to create detailed 3D models, simulate procedures, and identify optimal surgical approaches. This helps surgeons anticipate challenges and plan interventions more effectively.
9. What is the future of AI in cardiac surgery?
The future includes cognitive surgical assistants, holographic visualization, nanotechnology-based sensors, and integration with robotics and genomics. These innovations will further enhance precision, personalization, and patient outcomes.
10. How can healthcare providers start implementing AI?
Providers should begin with pilot programs in specific areas, invest in infrastructure and training, and collaborate with technology partners. Gradual integration ensures smooth adoption while building expertise and demonstrating value.
Conclusion
By embracing AI-driven personalized surgery, healthcare providers can elevate patient care to unprecedented levels of precision and personalization. The future belongs to those who act now—leveraging AI’s power to transform cardiac care and lead the way in innovation. Visit CardiPerf.com today to learn more about how AI can revolutionize your practice.