EBCP Anatomy and Pathophysiology MCQ Exam
Exam Overview
This exam consists of 80 multiple-choice questions (MCQs) divided into two sections:
- Section A: Anatomy and Physiology (40 MCQs)
- Section B: Pathophysiology (40 MCQs)
Each question has a 30-second timer. If you do not answer within 30 seconds, the exam will automatically proceed to the next question, and no marks will be awarded. Click ‘Next’ to proceed or ‘Submit’ on the final question to view results.
Introduction to EBCP Anatomy and Pathophysiology
The European Board of Cardiovascular Perfusion (EBCP) establishes rigorous standards for perfusion education and practice across Europe, with anatomy and pathophysiology forming the foundational knowledge base for every cardiac perfusionist. For the entire cardiac surgery team—including perfusionists, assistants, autotransfusionists, ECMO specialists, cardiac surgeons, and anesthesiologists—mastering these fundamental disciplines directly impacts patient outcomes during complex procedures involving cardiopulmonary bypass (CPB). This comprehensive guide explores the essential anatomical and pathophysiological concepts that underpin safe and effective perfusion practice, aligned with EBCP certification requirements and recent guideline updates.
The EBCP recognizes that perfusionists are specialized healthcare professionals responsible for operating heart-lung machines and other circulatory assist devices, managing patients’ physiological status during cardiac surgeries, and providing extracorporeal support in ICUs and emergency settings. In each of these roles, precise understanding of how anatomical variations and pathophysiological processes affect patient responses to extracorporeal circulation is crucial for both routine management and crisis intervention.
Foundations of Cardiovascular Anatomy and Physiology for Perfusionists
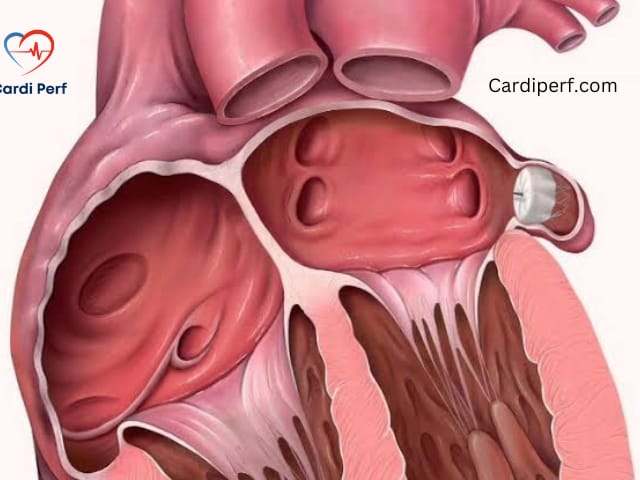
Cardiac Anatomy Relevant to Perfusion
The perfusionist’s understanding of cardiac anatomy must extend beyond basic structure to encompass the functional relationships that directly impact cannulation, drainage, and myocardial protection. Key anatomical considerations include:
- Chamber relationships and great vessel orientation that guide venous and arterial cannulation placement
- Coronary artery distribution patterns that determine myocardial protection strategies
- Cardiac venous drainage relevant to cardioplegia delivery
- Structural variations that may complicate bypass establishment
Vascular Anatomy and Cannulation Sites
Aortic arch branches, venae cavae, and femoral vessels represent critical access points for extracorporeal circulation. Perfusionists must understand the three-dimensional relationships between these structures and adjacent organs to anticipate potential complications. The EACTS/EACTA/EBCP guidelines provide specific recommendations regarding cannulation techniques based on anatomical considerations and patient-specific factors.
Circulatory Physiology During Bypass
The transition from native circulation to cardiopulmonary bypass represents a profound physiological shift that perfusionists must manage expertly. Understanding pressure-flow relationships, vascular resistance changes, and regional blood flow distribution allows for precise pump management. The mean arterial pressure targets outlined in EBCP guidelines reflect this sophisticated understanding of physiological principles during bypass.
Core Pathophysiological Principles in Perfusion Practice
Ischemia-Reperfusion Injury
Myocardial protection and organ preservation during cardiac surgery revolve around mitigating the cellular damage caused by ischemia-reperfusion. This complex pathophysiological process involves:
- Calcium-mediated injury to myocardial cells
- Inflammatory cascade activation following reperfusion
- Oxidative stress from reactive oxygen species generation
- Endothelial dysfunction impairing microvascular circulation
The EBCP guidelines detail specific strategies to counter these pathophysiological processes, including temperature management, cardioplegia composition, and reperfusion techniques.
Systemic Inflammatory Response to CPB
Contact of blood components with the non-endothelialized surface of the CPB circuit triggers a complex inflammatory cascade involving complement activation, leukocyte recruitment, and cytokine release. This systemic inflammatory response syndrome (SIRS) contributes to postoperative organ dysfunction and extends recovery time. Understanding these pathways enables perfusionists to implement strategies such as coated circuits, leucocyte filtration, and pharmacologic modulators to attenuate this response.
Hemostatic Alterations During Bypass
CPB induces profound changes in the coagulation system, platelet function, and fibrinolysis that create a delicate balance between bleeding and thrombosis. The EBCP emphasizes comprehensive anticoagulation management using activated clotting time (ACT) monitoring and individualized heparin protocols to maintain this balance. Pathophysiological understanding of how hypothermia, hemodilution, and contact activation affect hemostasis guides evidence-based transfusion and anticoagulation reversal practices.
Integration of Anatomy and Pathophysiology in Clinical Perfusion
Oxygen Transport Physiology and the Oxyhemoglobin Dissociation Curve
The oxyhemoglobin dissociation curve represents a fundamental physiological concept that perfusionists manipulate during CPB to optimize tissue oxygenation. This sigmoidal relationship between oxygen saturation and partial pressure is influenced by several factors that perfusionists control or monitor during bypass:
Table: Factors Affecting Oxygen-Hemoglobin Affinity
| Factor | Effect on Curve | Clinical Relevance in Perfusion |
|---|---|---|
| Temperature | Increased temp → Right shift | Active cooling increases O₂ affinity |
| pH | Decreased pH → Right shift | Acidosis promotes O₂ unloading |
| pCO₂ | Increased CO₂ → Right shift | CO₂ flush affects O₂ binding |
| 2,3-DPG | Decreased 2,3-DPG → Left shift | Stored blood has reduced 2,3-DPG |
The Bohr effect (influence of CO₂ and pH on oxygen binding) and Haldane effect (influence of oxygenation on CO₂ transport) work in concert to facilitate oxygen delivery to tissues and carbon dioxide removal. Perfusionists apply these principles when managing gas flow rates, sweep ratios, and acid-base balance during CPB.
Cerebral Physiology and Protection Strategies
Understanding cerebral vascular anatomy and autoregulatory physiology is essential for preventing neurological complications during CPB. The EBCP guidelines emphasize non-invasive cerebral monitoring techniques including near-infrared spectroscopy (NIRS) to detect deviations from normal physiological parameters. Perfusionists integrate knowledge of circle of Willis circulation, cerebral perfusion pressure thresholds, and temperature effects on cerebral metabolism to maintain neurological integrity during bypass.
Myocardial Energy Metabolism and Protection
The pathophysiology of myocardial ischemia informs cardioplegia strategies that perfusionists implement during aortic cross-clamping. The heart’s nearly exclusive reliance on aerobic metabolism under normal conditions shifts to anaerobic pathways during ischemia, with rapid depletion of high-energy phosphates and accumulation of harmful metabolites. Understanding these metabolic pathways allows perfusionists to customize cardioplegia composition, delivery temperature, and dosing intervals to maximize myocardial protection.

EBCP Examination Preparation: Anatomy and Pathophysiology Focus
Key Content Areas for EBCP Certification
The EBCP certification examination dedicates significant attention to anatomy and pathophysiology, with these topics comprising substantial portions of the Foundations in Cardiovascular Science section. The mock EB-CCP exam structure includes:
- 80 multiple-choice questions specifically on anatomy and pathophysiology
- 40 MCQs focused on anatomical concepts
- 40 MCQs addressing pathophysiological principles
This comprehensive coverage reflects the importance the EBCP places on foundational scientific knowledge as the basis for clinical decision-making.
Effective Study Strategies for Perfusion Teams
Successful preparation for EBCP certification requires a systematic approach to mastering the extensive anatomy and pathophysiology curriculum:
- Integrate clinical correlations between anatomical structures and perfusion techniques
- Focus on high-yield pathophysiological processes commonly encountered in cardiac surgery
- Utilize the EB-CCP mock exam to identify knowledge gaps and improve test-taking stamina
- Form multidisciplinary study groups to leverage different perspectives within the cardiac surgery team
Table: EBCP Exam Section Overview
| Exam Section | Question Count | Primary Focus Areas |
|---|---|---|
| Foundations in Cardiovascular Science | 80 MCQs | Basic sciences, anatomy, pathophysiology |
| Pharmacology and Physiology in Perfusion | 60 MCQs | Pharmacology, physiology, hematology |
| Cardiopulmonary Bypass Principles | 100 MCQs | CPB management, anticoagulation, organ protection |
| CPB Technology and Techniques | 40 MCQs | HLM components, cannulation techniques |
| Clinical Applications | 20 MCQs | Specific patient populations, patient management |
Advanced Considerations for the Modern Perfusion Practice
Emerging Technologies and Techniques
The EBCP guideline updates incorporate new sections on tubing materials, neuromonitoring, organ protection strategies, and blood purification techniques that reflect evolving understanding of pathophysiology during CPB. Perfusionists must maintain awareness of how anatomical variations influence the application of these new technologies and how pathophysiological responses might differ with their implementation.
Interprofessional Collaboration in Anatomical Assessment
Effective cardiac surgery teams leverage the collective anatomical expertise of each member. Surgeons provide direct visualization of cardiac structures, anesthesiologists contribute functional physiological assessment through transesophageal echocardiography, and perfusionists integrate these perspectives with their understanding of extracorporeal support implications. This collaborative approach ensures comprehensive patient assessment and management based on shared anatomical and pathophysiological knowledge.
Quality Improvement Through Pathophysiological Understanding
Analyzing perfusion-related adverse events through a pathophysiological lens enables targeted quality improvement initiatives. Understanding the anatomical reasons for cannulation malposition or the physiological basis for inadequate tissue perfusion allows for systematic protocol refinement rather than anecdotal problem-solving. The EBCP emphasizes this scientific approach to perfusion practice through its guidelines and certification standards.
Conclusion: Excellence in Perfusion Through Mastery of Fundamentals
For cardiac perfusionists and the entire surgical team, deep understanding of EBCP anatomy and pathophysiology remains the cornerstone of safe, effective patient care during extracorporeal circulation. As the field continues to evolve with new technologies and techniques, this foundational knowledge provides the framework for integrating innovations into clinical practice while maintaining the highest standards of patient safety.
The EBCP certification process validates this essential knowledge, ensuring that perfusion professionals across Europe possess the anatomical expertise and pathophysiological insight necessary to manage the complex physiological alterations induced by cardiopulmonary bypass. Through continued emphasis on these fundamental disciplines, perfusionists can optimize patient outcomes while advancing the science of extracorporeal circulation.
For the latest EBCP guidelines and updates, visit the official European Board of Cardiovascular Perfusion website at www.ebcp.eu
Of course! Here are 10 FAQs about “EBCP anatomy and pathophysiology,” tailored for the professional audience of cardiperf.com.
10 FAQs on EBCP Anatomy and Pathophysiology for Cardiac Perfusion Professionals
1. Why is a deep understanding of anatomy and pathophysiology so heavily emphasized in the EBCP certification?
For perfusionists, the heart-lung machine is an artificial physiology station. Your understanding of native anatomy and pathophysiology is what allows you to safely manage the patient’s transition onto and off of bypass. The EBCP tests this rigorously because it’s the foundation for troubleshooting intra-operative crises, optimizing cardioplegia delivery, and ensuring organ protection.
2. What are the highest-yield anatomical areas for a perfusionist to master for the EBCP exam?
Focus on the functional anatomy that directly impacts perfusion:
- Coronary Circulation: Dominance (right vs. left), sinus node artery origin, and coronary sinus anatomy for cardioplegia.
- Aortic Arch & Great Vessels: Variations that affect arterial cannulation and cerebral perfusion strategies.
- Right Heart & Venous System: Understanding thebesian venous drainage, SVC/IVC positioning, and how it relates to venous cannulation and drainage.
3. How does pathophysiology inform the management of the systemic inflammatory response (SIRS) during CPB?
CPB circuit contact activates complement, neutrophils, and the coagulation cascade, leading to capillary leak and end-organ dysfunction. Understanding this pathophysiological cascade is why we employ specific countermeasures: heparin-coated circuits, leukocyte-depleting filters, and targeted pharmacologic interventions to mitigate the inflammatory response.
4. What is the pathophysiological rationale behind different cardioplegia strategies (e.g., blood vs. crystalloid, antegrade vs. retrograde)?
This directly links anatomy to pathophysiology. Antegrade delivery relies on patent coronary arteries, while retrograde via the coronary sinus protects areas with coronary artery disease but has variable right ventricular distribution. Blood cardioplegia provides oxygen and buffers acidosis, while crystalloid causes less hemodilution. The choice is a physiological compromise based on the patient’s specific pathophysiology.
5. From a perfusionist’s view, what is the pathophysiology of ischemia-reperfusion injury?
It’s a two-phase process. During ischemia, ATP depletion and anaerobic metabolism lead to cellular acidosis. Upon reperfusion, the sudden influx of oxygen creates a burst of reactive oxygen species (ROS), calcium overload, and intense inflammatory activation, causing myocardial stunning and apoptosis. Our management of reperfusion pressure and composition aims to blunt this injury.
6. How does the pathophysiology of hemodilution on CPB impact my clinical decision-making?
Hemodilution decreases blood viscosity and oxygen-carrying capacity. The pathophysiology involves a balance: reduced viscosity improves microvascular flow but lowered hematocrit can impair oxygen delivery. This knowledge guides your decisions on priming volume, acceptable hematocrit thresholds, and the use of ultrafiltration to manage this balance.
7. What specific anatomical knowledge is critical for managing VA-ECMO as an ECMO specialist?
For peripheral VA-ECMO, understanding the femoral artery and vein anatomy relative to the bifurcation of the aorta and inferior vena cava is crucial. This knowledge prevents complications like limb ischemia (requiring a distal perfusion catheter) and Harlequin syndrome (inadequate cerebral oxygenation), which are direct consequences of cannula placement and patient anatomy.
8. How does the pathophysiology of hemostasis alter during CPB, and how does that guide anticoagulation management?
CPB creates a perfect storm for coagulopathy: hemodilution of clotting factors, hypothermia impairing enzyme function, platelet activation and consumption by the circuit, and fibrinolysis activation. This is why we cannot rely on standard heparin protocols alone. We use ACT monitoring and increasingly, viscoelastic testing (TEG/ROTEM) to guide targeted transfusion and anticoagulation reversal based on the specific pathophysiology.
9. As an autotransfusionist, how does pathophysiology relate to processing salvaged blood?
Salvaged blood is traumatized; it contains activated platelets, inflammatory mediators, free hemoglobin, and debris. Understanding this pathophysiology is why we wash the blood with saline—to remove these potentially harmful elements before reinfusion, preventing further activation of the patient’s inflammatory and coagulation systems.
10. What are the key cerebral physiological principles a perfusionist must monitor to prevent neurological injury?
The brain’s autoregulation curve (maintaining constant flow between ~50-150 mmHg MAP) is fundamental. During CPB, this curve can shift. We use cerebral oximetry (NIRS) to monitor regional oxygenation, understanding that embolic load (air, debris), MAP, PaCO2 (which affects cerebral vascular resistance), and temperature are the primary levers we control to protect the brain.